Providence Saint John’s Health Center and the Margie Petersen Breast Center
Cancer care is rarely straightforward, but every so often a case reminds us just how essential teamwork, coordinated diagnostics, and human-centered support truly are.
Her five physicians at Providence Saint John’s in the video below share this case because it reflects the power of a comprehensive, multidisciplinary model of care.
A Lump That Started an Unexpected Diagnostic Journey
Valerie first came to the Margie Petersen Breast Center after feeling a lump beneath her arm. For many patients, such a finding is frightening but often benign. In this case, it was the critical first clue.
Further evaluation revealed two distinct breast cancers in the same breast:

HER2-Positive Breast Cancer
- Aggressive and fast-growing
- Had already spread to at least one lymph node
- Required immediate systemic therapy
- ER-Positive Breast Cancer
Estrogen Positive Breast Cancer
- Slow growing
- Confined to the breast
- Treated surgically after chemotherapy
“She actually had two different breast cancers in her breast. One of them — the more aggressive HER2-positive one — had gone to the lymph node.”
–Parvin Peddi, MD
Because HER2-positive disease can spread early, the team proceeded with a whole-body PET scan — a decision that ultimately uncovered two more abnormalities.
A Full Body PET Scan Reveals Two More Masses
The PET scan identified:
- A renal mass
- An ovarian mass
These findings created immediate concern. Were these new cancers? Or had the HER2-positive breast cancer spread beyond the breast and lymph nodes?
“Because one cancer had already gone to the lymph node, we couldn’t assume the kidney or ovary were benign. They could have been metastatic or completely different cancers. We had to treat each one until proven otherwise.”
This marked a turning point in Valerie’s care — shifting from a single diagnosis to a complex multidisciplinary evaluation.
Treating the Most Urgent Threat First
HER2-positive breast cancer can be highly responsive to modern therapy. Valerie began multi-agent chemotherapy combined with HER2-targeted treatment.
Dr. Peddi emphasized the benefit of treating upfront:
After several months of therapy, breast surgical oncologist Dr. Janie Grumley performed Valerie’s breast-conserving surgery. The results were extraordinary.
“The more aggressive cancer was gone — no trace of it in the breast or lymph node. That’s the best response we can hope for,” Dr. Grumley shared.
The smaller tumor was completely removed at surgery.
A Third Cancer Revealed: The Renal Mass
Next, attention turned to the kidney mass. Biopsy results were inconclusive — not unusual for renal tumors — so urologic surgeon Dr. Jennifer Linehan evaluated the lesion further.
She explained how kidney cancers often behave:
Once Valerie completed her breast surgery and was safe to proceed, Dr. Linehan performed a robotic partial nephrectomy, removing the mass while preserving more than 85% of her kidney.
Pathology confirmed what the team had suspected: The kidney mass was a third, completely separate primary cancer — not metastasis.
This significantly changed the patient’s long-term outlook.
Clarifying the Ovarian Mass
Still, Dr. Park emphasized the importance of certainty:
“Given her complex oncologic history, we didn’t want to leave any potential stones unturned.”
She performed a minimally invasive laparoscopic removal. Pathology confirmed a benign fibrothecoma — the final missing piece of the diagnostic puzzle.
Supporting the Whole Person Through a Complex Journey
Undergoing surgery or treatment for even one cancer is emotionally taxing. Learning of three separate cancers over a short period can be overwhelming.
That’s when psycho-oncologist Dr. Shanthi Gowrinathan joined Valerie’s care team. She explained the psychological burden of multi-stage treatment:
Dr. Gowrinathan highlighted an often-overlooked aspect of cancer care:
“People think they’re supposed to just live with insomnia, appetite changes, pain, or emotional distress. These are treatable issues — and addressing them is part of the therapeutic process.”
Through integrated supportive care, the team helped Valerie regain emotional grounding and resilience during recovery.
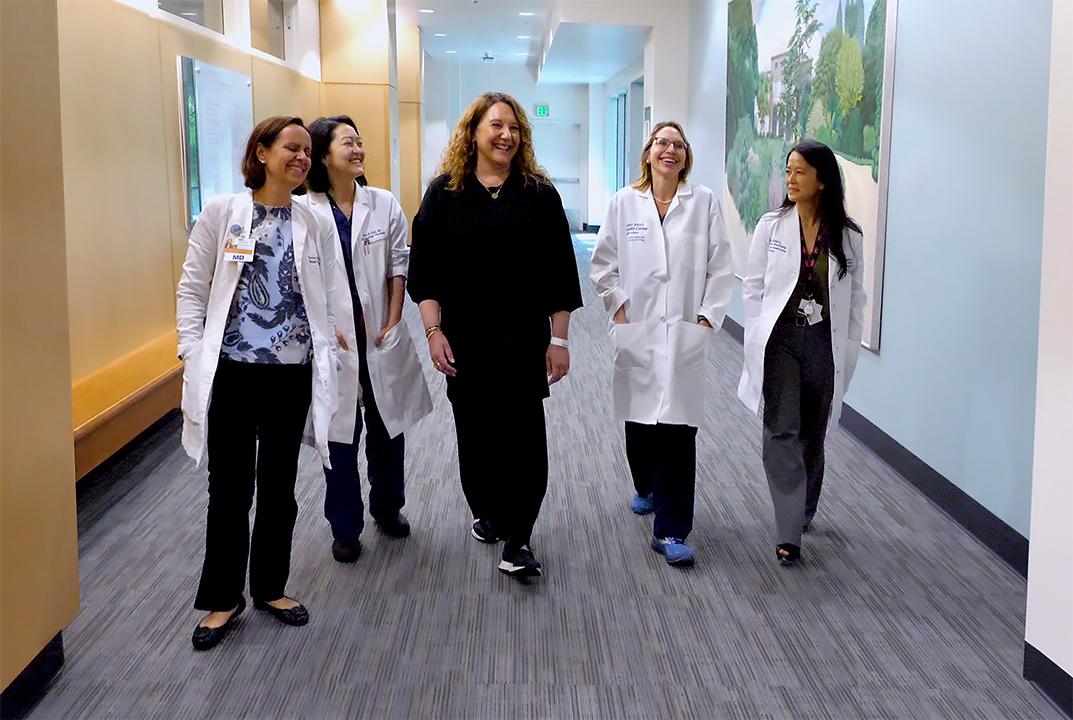
5 Oncologists Discuss Valerie’s Case & A Multi-Disciplinary Approach
Janie Grumley, MD, Jennifer Linehan, MD, Parvin Peddi, MD, Hyo Park, MD, Shanthi Gowrinathan, MD at Saint John’s Cancer Institute
What This Case Teaches Us
This uncommon case illustrates several important principles of modern cancer care:
- Multiple synchronous cancers are possible — and easy to misinterpret. Careful imaging, pathology, and timing prevented misdiagnosis.
- HER2-positive breast cancer can mask other cancers. Because it spreads early, any additional mass must be evaluated as possible metastasis.
- Kidney cancer often goes unnoticed. Many renal tumors are silent until discovered incidentally.
- Co-located multidisciplinary teams accelerate care. Having oncologists, surgeons, urologists, gynecologic specialists, and supportive care providers under one roof allowed rapid decision-making.
- Emotional recovery is as important as medical recovery. Cancer treatment affects the mind, body, identity, and daily functioning — and expert support must be part of care.
A Unified Team With a Unified Goal
Valerie’s journey underscores the importance of comprehensive cancer care built around collaboration, communication, and compassion.
Physicians across five specialties coordinated seamlessly to diagnose, sequence, and treat multiple cancers, all while ensuring that the patient’s emotional and psychological well-being remained central.
This is the strength of the Providence Saint John’s model: multidisciplinary care that treats the whole person — not just the disease.
Valerie Shares Her Journey, How She Managed Her Multi-cancer Diagnosis
Blog, Video (21:35): Multiple Primary Malignancies Found in the Breasts and Kidney