There’s more to know about Bladder Cancer
Bladder cancer is different than other cancers in that there is no known genetic connection between family members or generation to generation. However, certain conditions in the body may evolve which can result in developing cancer later in life but are unique person-to-person. The common factors are chemical exposure and smoking, where Dr. Linehan emphasizes the danger and possibility of developing tumors as a result.
Approximately 200,000 patients a year are newly diagnosed with bladder cancer, while men are affected more than women, likely due to increased smoking. To help patients understand bladder cancer and their diagnosis, Dr. Linehan explains the different types of bladder cancer to her patients, easing their anxieties and fears. In the video, Dr. Linehan also discusses clinical trials, bladder preservation, and cancer prevention.
Signs of Bladder Cancer and Diagnosis
Aside from surgical removal of smaller tumors during endoscopy, treatments are bladder-specific, including the use of chemical washes (liquid treatments that temporarily fills the bladder) that deliver chemotherapy or BCG (Bacillus Calmette-Guérin—an immunotherapy drug), which improves immune response signaling. More advanced bladder cancer treatment may require minimally invasive techniques such as using a robotics system. Dr. Linehan is an expert bladder, kidney, and ureter reconstruction surgeon.
If you see blood in the urine…get checked out with a CAT scan, camera in the bladder, and possibly one of the 5 urine tests that I talked about…
– Jennifer Linehan, MD
Bladder Cancer Awareness: What to look for
Dr. Jennifer Linehan explains all things bladder cancer, diagnosis, and treatment.
Treatment
A biopsy is needed to determine bladder cancer, identify if it is high- or low-grade, and subsequent treatments. A catheter is used to deliver chemotherapy to treat tumors on the inside of the bladder, which is well tolerated by patients, according to Dr. Linehan. This treatment lasts for 6 weeks, requiring patients one weekly visit each week. BCG is one such treatment that is also applied as a bladder wash. Dr. Linehan maintains that there is still a significant percentage of cases that can recur, therefore continuous observation is needed.
A lot of patients come see me because they want to pursue bladder sparing protocols.
– Jennifer Linehan, MD
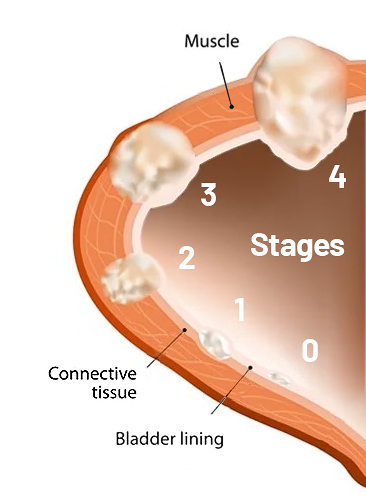
Some bladder cancers invade the muscle wall, which changes how it is treated. In many cases, chemotherapy and bladder removal are necessary (cystectomy). In bladder-sparing approaches, chemotherapy and radiation may be the suggested method of treatment. This approach helps to maintain bladder function. Therefore, a careful diagnosis is needed (looking for high-grade cancer) to know if it is safer to remove the bladder entirely. If the bladder is removed, a new bladder (neobladder) is constructed using tissues from the patient.
Bladder Treatment Breakthrough

Saint John’s Health Center uses Blue Light CystoscopyTM to find bladder cancer that is more difficult to detect. By using a special fluid in the bladder that glows bright pink under blue light, the smallest of cancer sites become immediately visible. This allows us to treat those sites sooner and avoid the possibility of additional treatments in the near future.
Learn more and watch a video about Blue Light Cystoscopy for bladder cancer.
What to do and know to help prevent bladder cancer
Dr. Linehan provides several examples to help reduce your risk of bladder cancer. As always, you will want to develop a routine process with your doctor so that changes or new occurrences can be identified and treated sooner than later.
- Stop smoking (tobacco use).
- Establish regular urinalysis screening to detect blood in the urine of at-risk individuals.
- Avoid certain herbs that contain aristolochic acid (Aristolochia fang chi).
- Avoid exposure to benzine-related chemicals and artificial dyes, which remain in use today commercially to dye silk, wool, and other proteinaceous fibers.
- Bladder cancer is not transferred genetically from generation to generation.
Contact Dr. Linehan today if you have questions about bladder cancer and related urologic conditions.
Learn More:
- Physician’s Bio: https://www.saintjohnscancer.org/about-us/people/jennifer-linehan/
- Bladder Cancer Conditions & Treatment: https://www.saintjohnscancer.org/urology/conditions/bladder-cancer/
- Urology Center of Excellence: https://www.saintjohnscancer.org/urology/
#melanomaawareness #cancerresearch