Two Clinical Trials and a Team of Specialists Later, Kevin and Candice Discuss Brain Cancer, Together
“Don’t Google it,” mentions Kevin Hodges in his testimonial. 4 years ago today, Kevin was diagnosed with a 3-centimeter glioblastoma (GBM) tumor during the height of the pandemic. His prognosis, 18 months to live. His outcome outperformed the life expectancy of those with GBM by 3 times. “I feel amazing. I’m not going to lie; I feel good. If you get upset and you get depressed about it, it kind of doesn’t help. It’s been shown to not help you,” says Kevin.
Besides the relentless support Kevin received from his wife, Candice, he may be an outlier for one reason. Kevin found a multidisciplinary team of specialists who understood how to treat glioblastoma by finding and putting Kevin on the correct clinical trial at the right time. “You have to be able to pick the right agent at the right time, and that comes with knowing how to treat these kinds of cancers,” explains Dr. Naveed Wagle, one of Kevin’s medical neuro-oncologists.
Glioblastomas are malignant (cancerous) grade 4 tumors that arise as a grade 4 with no evidence of a lower-grade precursor. They are typically found in the frontal lobe, followed by the temporal, parietal, and occipital lobes. Symptoms include seizures, severe headaches, memory and language problems. Changes in personality and behavior, muscle weakness and paralysis, fatigue, issues with coordination, and speech, vision, or hearing problems are also common.
Kevin presented with severe migraines, which lasted months. “I was taking way too much ibuprofen that was probably healthy for me.” Kevin’s ability to articulate words disappeared entirely following a trip to an emergency room at 3 am. “He was unable to answer basic questions: What is your birthday? What is your age? etc.,” recalls Candice.
Kevin’s journey with cancer included three craniotomies (brain surgeries), a standard of care, and two clinical trials. Of which, the 2nd clinical trial was his Hail Mary, OKN007 (a drug trial). It was a long journey of commitment and dedication deserving of praise because no one is guaranteed life, as Kevin explains, but with support and care, you can give yourself a fighting chance. His prognosis may have looked different if not for those who supported his healing process. Today, Kevin has been off treatment for 6 months and we are so elated for him, his wife, and his team of experts for going the distance. Kevin can now transition to the next phase of his journey, helping others. “I knew you could do it,” Candice says to Kevin at the conclusion of his video testimonial.
“I think hope is an important part of any journey but, particularly in cancer.”
– Dr. Naveed Wagle
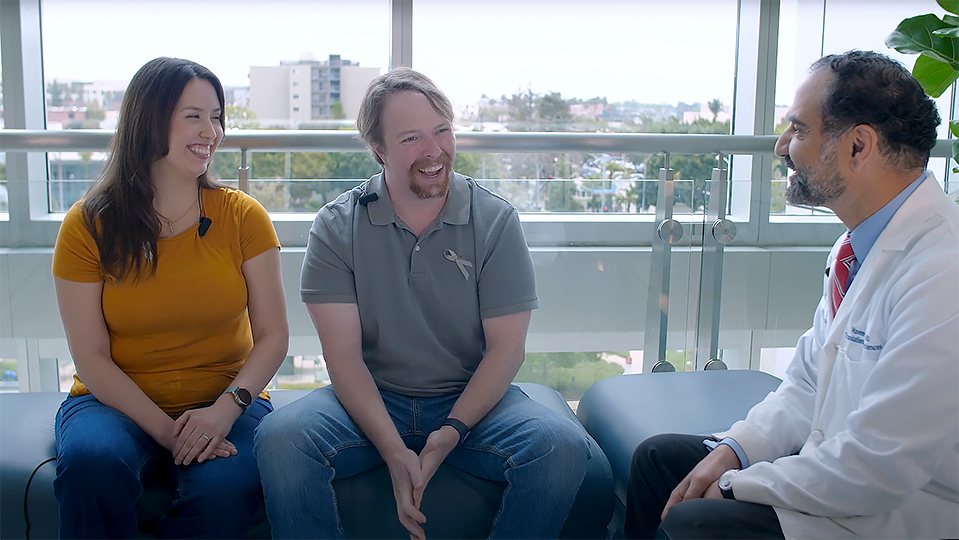
Listen to Kevin, Candice, Dr. Wagle, and Dr. Sharma Discuss this Incredible Case!
Kevin and Candice Hodges sit alongside health care professionals, Dr. Wagle, and Dr. Akansha Sharma, May 2024.
Why are Glioblastomas So Difficult to Treat?
- There are limited treatments other than standard-of-care (chemotherapy & radiation) after surgery.
- There are no screening methods other than accidental medical discovery: symptoms are all you have, and some tumors have no symptoms.
- It’s an aggressive cancer—it grows quickly, consuming space and invading nearby brain tissue.
- There are limited clinical trials available.
- Getting medicine past the blood-brain barrier to kill the cancer requires highly advanced treatment.
- The biology of the tumor is uncommon.
“The clinical trial, I say, was great. I mean having that option was what we wanted, and I would be way more scared if they said, there’s nothing else we can do.”
– Candice Hodges
For Kevin and Candice, seeking specialized care lifted many burdens that Candice mentioned a few times as “eye opening,” especially the part where they considered Candice’s needs besides Kevin’s. “Another huge difference between this group and any other group is they not only offer care for the patient, which is their number one priority, but they were offering me care…There’s a lot of things that go on while your loved one is sick…Bills still got to get paid. Things have to get done around the house and things have to keep moving, and they definitely support you in anything that you need.”
Elevating the Standard of Care
Between Saint John’s Health Center’s (SJHC) state-of-the-art technology, Saint John’s Cancer Institute’s (SJCI) innovative clinical trials, Pacific Neuro Institute’s (PNI) brain health and well-being programs, and how they support each other to develop individualized care plans for their patients, it is difficult to find one place to support a multipronged approach to health care. Fortunately, this capability allows us to provide personalized support for our patients and their family members, elevating the standards of care.
“You just have to stay focused and go looking for the help because it’s out there.”
– Candice Hodges
“I think it’s very important for multiple reasons. One is patient care, so another side to multidisciplinary is that a lot of times there isn’t a single way forward. Right? So, you want to pick the best option for an individual person. Sometimes that involves coordinating with the surgeons, coordinating with the radiation doctors, coordinating with the social worker, so you get the right thing at the right time. And a lot of times here, what we’re able to do is sit down and talk about that with the clinicians—the people that are involved in your care, so that we’re all on the same page,” explains Dr. Wagle.
In summary, it’s not just access to clinical trials, it’s the foresight of engaging in the right trial at the right time even if the normal course of treatment is underway.
What’s next for Kevin and Candice? They want to help others diagnosed with glioblastoma and finally start a family of their own.
Takeaways from Kevin’s Journey:
- A clinical trial may be a great option in addition to your care, and not as a last resort.
- Advocate for yourself (ask questions), and then learn to trust those caring for you.
- Find a team of experts who will work seamlessly together on your behalf.
- Have a positive attitude because this may carry you further, considering the severity of the journey.
“You quickly learn that with glioblastomas you need help. Ask for help.”
– Candice Hodges
Meet Kevin’s Team of Experts
 |
 |
 |
|
|
Garni Barkhoudarian, MD
Neurosurgeon Director, Skull Base Microdissection Anatomy Laboratory |
Santosh Kesari, MD, Chair, Department of Translational Neurosciences; Director of Neuro-oncology
|
Naveed Wagle, MD, Translational Neurosciences, Neuro-Oncology, Pacific Brain Tumor Center
|
Akanksha Sharma, MD, Neuro-Oncology, Translational Neurosciences
|
Learn more about the Pacific Neuroscience Institute.
Visit Pacificneuroscienceinstitute.org.