Squamous Cell Carcinoma cases are reviewed by a multi-disciplinary tumor board to personalize effective treatment plans at Saint John’s Cancer Institute and Health Center.
What is Squamous Cell Cancer?
Squamous Cell Carcinoma (SCC) is the second most common form of skin cancer that typically develops from chronic sun-exposed areas of your body. SCC manifests as uncontrolled growth of cells in the epidermis though is typically far less aggressive as melanoma. The growth of cells can become disfiguring and sometimes deadly if untreated. Squamous cell carcinomas are at least twice as frequent in men as in women and are most often seen in individuals in their 70s.
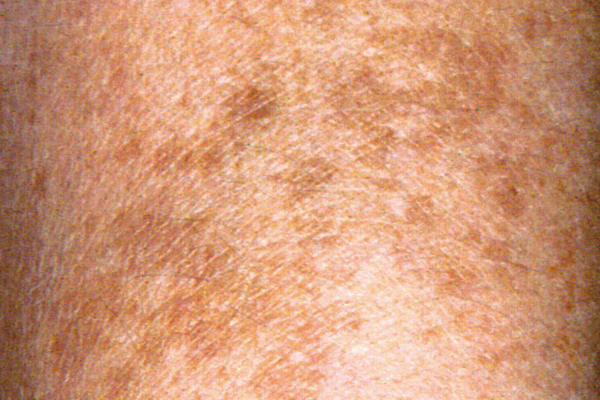
What does a Squamous Cell Carcinoma Look Like?
Squamous cell cancers of the skin can commonly present as:
- Scaly red patches
- Open sores
- Elevated growths with a central depression
- Warts
- They may crust or bleed.
The 5 Stages of Squamous Cell Skin Cancer
Most squamous cell cancer of the skin present as Stage 0 or 1. This gives doctors greater opportunities to treat the cancer early, which may be final and curative.
Stage 0
Stage 0 is not considered invasive cancer. Abnormal cells exist only in the upper layer of the skin.
Stage 1 and 2
These stages are determined by the size of cancer and if high-risk features exist.
Stage 3
This stage indicates spread to areas below the skin, such as the lymph nodes or other structures like muscle, bone, or cartilage
Stage 4
Stage 4 SCC indicates cancer spread to distant sites, such as organs, distant lymph nodes and other structures.
Risk Factors
SCC is Mainly Caused by Cumulative UV Exposure Over the Course of a Lifetime.
Previous Skin Cancer
If you have had squamous cell carcinoma, a common type of skin cancer that tends not to spread, you may be more likely to develop a squamous cell skin carcinoma.
Immune Impairment
Reduced immune response can also create conditions that can lead to greater occurrence of SCC. Chronic infections, skin inflammation, HIV and other immune deficiency diseases, as well as chemotherapy and anti-rejection drugs used in organ transplantation can all elevate squamous cell skin carcinoma
Genetics
Occasionally, squamous cell carcinomas arise spontaneously on what appears to be normal, healthy skin. Some researchers believe the tendency to develop these cancers can be inherited. Anyone with an inherited, highly UV-sensitive condition such as xeroderma pigmentosum, may present with greater occurrences.
SCCs may occur on all areas of the body including the mucous membranes and genitals, but are most common in areas frequently exposed to the sun:
- Ears
- Lower lip
- Face
- Bald scalp
- Neck
- Hands
- Arms
- Legs
Often, the skin in these areas will reveal signs of sun damage, such as wrinkling, patchiness, changes in pigmentation, and loss of skin elasticity, especially as with aging.
People who have the following features are at highest risk of developing squamous cell carcinoma:
- Fair/light colored skin
- Light hair
- Blue, green, or gray eyes
- Precancerous lesions (actinic keratosis, actinic cheiltis, leukoplakia and Bowen’s disease)
- Substantial sun exposure
- Previous BCC or SCC
- Chronic inflammatory skin conditions or chronic infections
Though these represent who is at most risk, anyone with a history of substantial sun exposure is at increased risk. Those whose occupations require long hours outside or who spend extended time in the sun are also at risk.
Squamous Cell Carcinoma Diagnosis
In order to diagnose squamous cell carcinoma of the skin, a biopsy is required.
Physical exam
Your doctor will examine the affected area of the skin to look for particular signs of squamous cell carcinoma. The exam will also include a review of your health history.
Biopsy
Your doctor will need to collect a small tissue sample of skin using a special tool to cut away some or all of the suspicious lesion. The type of skin biopsy performed will depend on your situation. After collection, the tissue is sent to a laboratory for genetic analysis.
Squamous Cell Carcinoma Treatment
SCCs that are detected and promptly removed at an early stage are almost always curable, causing minimal impact to the skin. However, if SCCs are left untreated, they may grow to the point of being very difficult to remove and treat.
A small percentage of SCC cases may metastasize to distant tissues and organs. Your doctor can determine if there is increased risk for metastasis and if you will need treatment beyond simple, localized excision. Fortunately, there are several effective ways to treat squamous cell carcinoma. The choice of treatment is based on the type, size, location, and depth of the tumor in the skin, and is dependent on your age and general health. Squamous cell carcinoma treatment is generally performed on an outpatient basis.
When seeking care for squamous cell carcinoma, the whole body is examined for lesions not just the affected area. A skin biopsy may be performed for suspicious moles to determine if cancer is present and which cancer it is. The type of skin biopsy performed will depend on the type and size of lesion.
A diagnosis of squamous cell carcinoma can only be confirmed with a biopsy. This process involves taking a small piece of the affected tissue and examining it in our laboratory. Additional tests may be needed. If cancer cells are present, treatment is required. Fortunately, there are several effective methods available.
Treatment options are based on:
- Type of cancer
- Size of the tumorous tissue
- Location of the BCC
- Depth of the tumor (does it extend to the dermis and beyond)
- The patient’s age and general health
- The likely cosmetic outcome of specific treatments
In many cases, a simple excision (surgical removal) can be curative. A dermatologist might perform this. A technique called Mohs surgery may be performed to maximize skin preservation, which requires a surgeon specialist. In some cases, other treatments including radiation or topical therapies may be considered.
Surgery
Surgical excision of the affected tissue removes the cancerous lesion and a surrounding margin of healthy skin. This helps to reduce the risk of recurrence. The extent of the margin is determined by microscopic examination to verify the absence of cancer cells in the surrounding margin. Surgery is typical for squamous cell carcinomas in areas where they are less likely to recur.
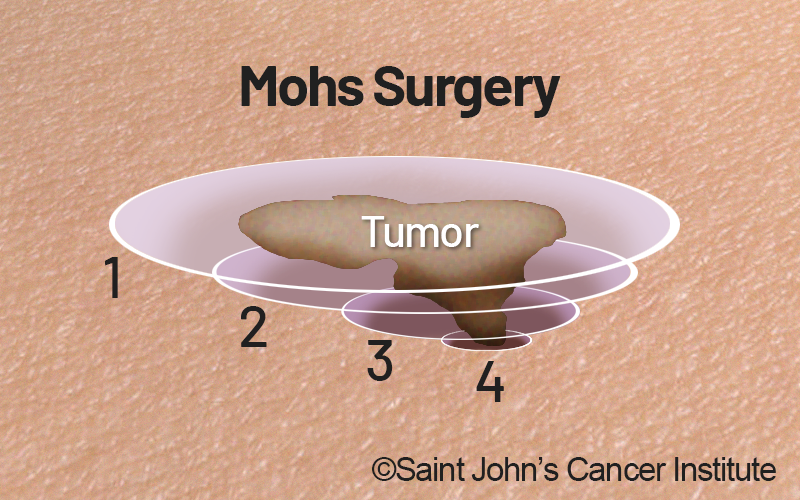
Mohs Surgery
Mohs surgery is a specific method of excision designed to conserve as much normal tissue as possible. During Mohs surgery, the cancer is removed layer by layer, which allows examination of each layer under a microscope until no abnormal cells remain. This guides the direction and depth of the surgery, thereby removing the entire growth while avoiding healthy skin. If your squamous cell carcinoma is larger and has an elevated risk of recurring, extends deeper, or is located on your face, Mohs surgery may be recommended.
If you are unable to undergo surgery, or if you have decided against having surgery, the oncologist may recommend other types of treatment.
Radiation therapy
Radiation therapy uses high-energy beams, such as X-rays and protons, that kill cancer cells by disrupting their DNA. By focusing the beams to the target area, therapeutic result is maximized while reducing side effects. Radiation therapy can be given after surgery to help reduce the chance of recurrence and may be used when surgery is not an option.
Freezing (Cryosurgery)
Some cases of squamous cell cancer can be treated entirely using liquid nitrogen, killing the cells by freezing them. This is particularly useful for treating smaller, superficial skin lesions, or when surgery is not an option. Freezing can also be combined with curettage treatment, which removes the surface of the skin cancer.
Topical treatments
Prescription creams and ointments are a viable option for small squamous cell carcinomas that are less deep and when surgery is not an option. Like other prescription medicines, it used as required by the treating physician.
Treatment for squamous cell carcinoma that spreads
It is rare for squamous cell carcinoma to spread (metastasize) to the lymph nodes and other areas of the body. If this occurs, however, there are treatments designed to help suppress cancer spread and its growth.
Targeted Therapy
Targeted drug therapy may be recommended by the oncologist and works by taking advantage of genetic and molecular flaws within cancer cells. By blocking the cancer’s ability to sustain itself, it shrinks and dies. Targeted therapy drugs may be considered after other treatments or when those treatments are not possible.
Chemotherapy
Chemotherapy drugs are designed to kill cancer cells. It might be an option when other treatments have not helped. Can be given orally, intravenously, or in other ways while doses are carefully selected to target the specific type and stage of the cancer.
Immunotherapy
Immunotherapy is also a drug treatment that works by helping the body fight cancer. Some cancer cells produce proteins that evade the immune system and therefore not attack the cancer. Immunotherapy drugs work by disrupting the process of cancer evasion.
How to Prevent Squamous cell Carcinoma
Chronic exposure to sun light is one of the highest risk factors in the development of squamous cell cancers.
Prevention methods include:
- Avoid the sun between 10AM to 4PM when UV radiation is the strongest.
- Avoid using tanning beds.
- Wear sun protective clothing and hats.
- Use a broad-spectrum sunscreen (30 SPF or greater) if outside for extended periods.
- See a dermatologist once a year for a head-to-toe skin examination.
For high-risk patients, research has shown that nicotinamide, a vitamin B3 supplement, reduced the rate of new squamous cell and squamous cell skin cancers by approximately 23% compared with placebo.
If you have questions regarding squamous cell carcinoma or would like an expert second opinion, please call today or click here to schedule an appointment.