Melanoma cases are reviewed by a multi-disciplinary tumor board at Saint John’s Cancer Institute and Health Center to personalize effective treatment plans.
What is Melanoma Skin Cancer?
Melanoma is an aggressive type of skin cancer. It develops in the cells that control our pigmentation (melanin). If your mole pigment has changed its’ color, shape, and size, this may be an indication to seek out medical advise. Excessive exposure to sunlight (ultraviolet radiation) increases the chances of developing skin cancer, and 1 in 5 people will be diagnosed with skin cancer at some point in their lifetime. More so, melanomas account for 3 percent of all skin cancers. Precautions to protect your skin should be taken your entire life.
Our knowledge of melanoma has led to significant breakthroughs including less invasive surgical techniques, targeted medical treatments options, and in-depth understanding of the scope of disease (such as brain metastasis and how to treat it). Our comprehensive approach includes the Sentinel Lymph Node Biopsy; a procedure pioneered by Saint John’s Cancer Institute. It has become the standard of care for treating melanoma surgically, worldwide.
Why is skin cancer so dangerous?
Melanomas frequently, and aggressively, invade other parts of the body because they travel through the bloodstream. Survivability of melanoma diminishes if it goes untreated. In recent decades, melanoma cases have increased in women under the age of 40, and is the main cause of death in women from ages 25 to 30. Early detection and treatment of melanoma often results in a cure. Other factors include location; did melanoma develop on the extremity or the stomach? Location of melanoma may increase how aggressively it spreads to other parts of the body.
How quickly can Melanoma spread?
Melanoma, one of the most aggressive forms of skin cancer, can spread rapidly if not detected and treated early. The speed at which melanoma spreads varies, depending on several factors such as the stage of the cancer, the thickness of the tumor, and the overall health of the individual. Unlike other types of skin cancer, such as basal cell carcinoma or squamous cell carcinoma, melanoma is particularly notorious for its ability to metastasize quickly to other parts of the body, including the lymph nodes, lungs, liver, brain, and bones.
Melanoma originates in the skin, and while its initial spread is often local, it can quickly invade nearby tissues or move to other skin areas and deeper into the body. Early detection and prompt treatment are crucial for preventing melanoma from spreading. Treatment options might involve surgery, immunotherapy, targeted therapy, or a combination of these methods, depending on the cancer’s stage. The stage of melanoma is a key factor in determining how quickly it can spread; in the early stages, melanoma may be confined to the skin, but in later stages, it can metastasize rapidly. Understanding the staging and seeking timely treatment is vital for controlling the spread of melanoma and improving survival rates.
Treating and surviving skin cancer starts with early detection.
Early Signs of Melanoma
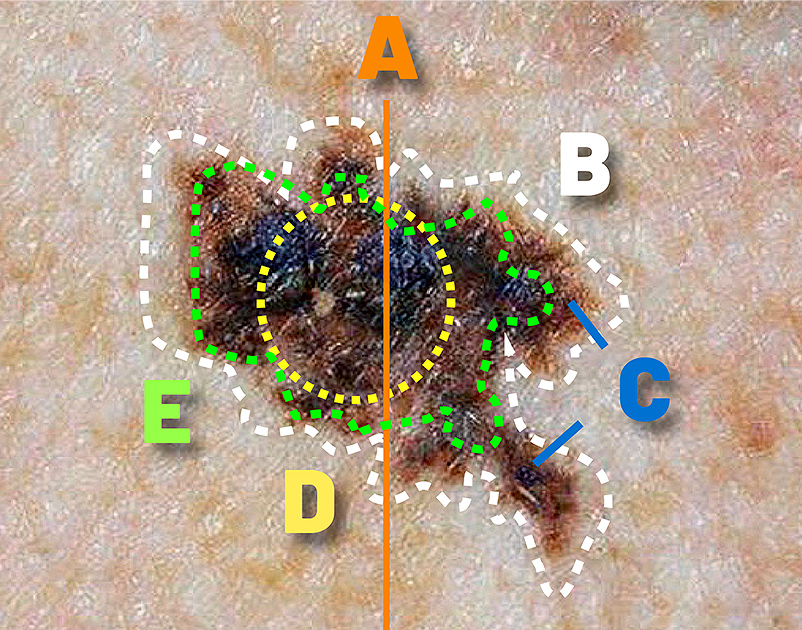
Skin cancer detection begins with observing the ABCDEs. This self-assessment method, A-B-C-D-E, is a straightforward way to identify early melanoma risk and take steps to prevent further skin damage.
Using ABCDE to find melanoma
B = Border (Is it ragged along the edges?)
C = Color (Are there many distinct colors or shades?)
D = Diameter (Is it above 6 millimeters or about 1/4 inches in size?)
E = Evolution and everything else (Are there any changes in color, size or look of the mole over time?)
Other signs may include
- Bleeding or crusting within or along its edges
- Variations of color on existing moles
- Development of a raised area of the skin
- Lesion (abnormal lump, bump, ulcer, sore, or colored area on the skin)
Tanner Deason’s Story: A Stage 4 melanoma patient with brain metastasis shares his treatment experience at Saint John’s. Learn more and watch his inspiring video (9:30). (A Chanced Discovery of Stage 4 Melanoma with Brain Metastasis)
Melanoma Risk Factors
Anything that increases your chance of getting melanoma is a risk factor. Sun exposure and related skin damage, especially having a history of peeling or blistering sunburns, are the primary risk factors for melanoma. Artificial sunlight from tanning beds causes the same risk for melanoma as natural sunlight, due to the use of ultraviolet radiation. Learn more about the effects of UV radiation and protecting the skin.
Considerations for Risk
- Having a previous diagnosis of melanoma
- Having many benign (non-cancerous) moles
- A family history of melanoma
- Atypical mole and diagnosis of melanoma syndrome (AMS)
- If you have AMS, you and your family members should be screened regularly
Not everyone with a risk factor is diagnosed with melanoma. Individuals are encouraged to visit their primary care doctor or a dermatologist if they have any concerns or suspicions about melanoma.
Contact the Saint John’s Cancer institute and Health Center if you:
- Have a light skin color with a greater sensitivity to the sun
- Have multiple moles that are irregular or have recently appeared
- Have a family history of melanoma
- Have a history of blistering sunburns or extended UV exposure
Melanomas on the arms and legs generally have a better prognosis than those on the head and neck or trunk. Mucosal melanomas (including the lips, mouth, or gums) have an overall poor prognosis, often because they are detected late.
“Our ongoing biomedical research combined with our surgical expertise is improving patients lives.”
Prognosis, Treatment, and Diagnosis
A team of experts will determine the stage of melanoma through biopsy and cancer progression, as being either stage 1, 2, 3, or 4, or somewhere in between. Surgery is still the most curative aspect of treating melanoma.
Diagnosis of melanoma is often performed by a simple skin exam followed by a biopsy. In some cases, additional imaging may be required. A skin examination is often performed first by a dermatologist, or primary care physician while a biopsy is conducted by an experienced oncologist and evaluated by a pathologist.
At Saint John’s Cancer Institute, our ability to collaborate with a team of melanoma experts is greatly respected. Our physicians who diagnose the extent of the disease work directly with scientists at the institute to identify the genetic attributes of cancer. This ensures a personalized plan by measuring how the cancer changes before, during, and after initial treatment. Treatments for melanoma may include radiation therapy, targeted therapy, and immunotherapy, which can be used independently, or together.
How is Melanoma Staging Determined?
Melanoma cancer staging is determined through a combination of factors that assess the extent of the cancer’s spread and its characteristics. The staging process is critical for guiding treatment decisions and predicting outcomes. Here’s how melanoma staging is typically determined:
1. Tumor Thickness (Breslow Depth)
The thickness of the melanoma, which is measured in millimeters, is one of the key factors in staging. This measurement shows how deeply the cancer has grown into your skin. Generally, the thicker the tumor, the higher the stage and the more serious it might be.
2. Ulceration
Ulceration means there’s a break or sore on the skin over the melanoma. If your melanoma is ulcerated, it’s considered more aggressive, which can place it in a higher stage.
3. Mitotic Rate
The mitotic rate is a measure of how quickly the cancer cells are dividing. A faster rate suggests a more aggressive melanoma, which could impact its stage.
4. Lymph Node Involvement
Doctors check whether the melanoma has spread to nearby lymph nodes. If it has, the stage is usually higher. This is an important factor because it shows that the cancer has started to move beyond the original spot.
5. Metastasis
Metastasis refers to whether the melanoma has spread to other parts of your body, like the lungs, liver, or brain. If it has spread to distant organs, it’s classified as stage IV, which is the most advanced stage.
6. Tumor Location
The location of the melanoma on your body also plays a role in staging. For instance, melanomas on the scalp, neck, or inside the mouth can be more serious and might be staged higher.
7. Sentinel Lymph Node Biopsy
In some cases, especially if your melanoma is thicker or has other high-risk features, your doctor might recommend a sentinel lymph node biopsy. This test checks if the cancer has spread to the lymph nodes and helps with accurate staging.
8. TNM System
Doctors use a system called the TNM system to help stage melanoma:
- T (Tumor): How thick the tumor is and whether it’s ulcerated.
- N (Node): Whether the cancer has spread to lymph nodes and how many are affected.
- M (Metastasis): Whether the cancer has spread to other parts of your body.
Biopsy for Melanoma Staging
Biopsies are great determinants for finding benign (non-cancerous) or malignant (cancerous) skin cancers.
If melanoma has been discovered after a review performed by a pathologist, a vast amount of information can be obtained about its specific genetic attributes through our sequencing lab. If the initial biopsy was performed by another organization, our pathologists can quickly provide a review or expert second opinion. There are many types of biopsies that are utilized to determine a diagnosis, including local excision biopsy, punch biopsy, and shave biopsy.
Results of the biopsy may reveal a diagnosis of:
- Benign (non-cancerous) growths such as moles, warts, and benign skin tumors
- Squamous cell carcinoma
- Basal cell carcinoma
- Melanoma
- Merkel Cell Carcinoma
Melanoma Cancer Stages
Staging may involve more than one number which requires an explanation from your oncologist. For example, Stage-3 melanoma is vastly different from melanoma with Level III invasion.
Stages 1 and 2
Early melanomas (Stages 1 and 2) are localized and have not advanced to other parts of the body. The lower, or earlier the stage, the more likely a patient will be cured of cancer.
Stage 3
Stage 3 melanoma occurs when the cancer cells have spread from the primary tumor site through the lymph nodes (small channels in the tissue). As a result, the tumor cells from the original location can be detected near the region of the primary melanoma. If melanoma spreads this way, the risk of it spreading further to other parts of the body becomes greater.
Stage 4
Stage 4 melanoma occurs when cancer cells have traveled through the body via the bloodstream or lymph vessels and have settled into other areas. These cancer cells are detectable in organs and other critical systems in addition to the lymphatic spread.
Know the difference of a comprehensive, multi-disciplinary approach.
Melanoma Treatments
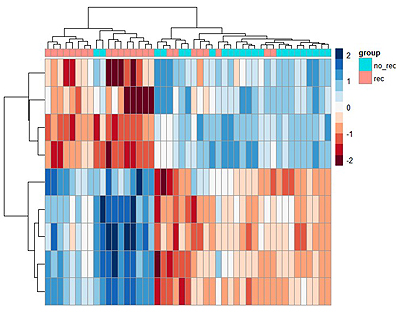
Treatments for melanoma are rapidly progressing because of clinical trials and biomedical research. Decades of melanoma research, biospecimen banking and data, have given our physicians a unique ability to treat cancer with innovative medical therapies. AI (Artificial Intelligence) has also enabled our researchers, allowing analysis of larger amounts of data, deeper comparisons and forecasting, and future treatment impact to develop new drug therapies with greater clinical accuracy for our patients. Collaboration with outside organizations and academia has also supported greater understanding of treatments as well.
Dermatologists trust the physicians at Saint John’s Cancer Institute and Health Center for our ability to identify and successfully treat melanomas. We can identify early signs of melanoma and provide a personalized care path proven to optimize outcomes. Complex cases, including Stage 3 and 4 cases with metastasis to the brain, are well documented, giving patients hope for a cure. Treatments for melanoma at Saint John’s Cancer Institute and Health Center has been compared to MD Anderson Cancer Center of Texas and Memorial Sloan Kettering in New York.

Surgery (Wide Local Excision)
Removal of cancerous tissues or gland (See Wide Local Excision for Treatment of Melanoma
- The main treatment options of most sarcomas
- Addresses the treatment area and a small portion of the surrounding area
- May be a final treatment for some tumors
- May involve removal of lymph nodes near the primary tumor
- Can be utilized with other types of treatment
Radiation
Focused beams of energy that disrupt tumor growth by damaging the DNA of the cancer (See Radiation Therapy for Melanoma
- Can be given before or after surgery, and in different ways
- Typically used in larger, higher-grade tumors
- Often used to treat an area where the cancer is likely to recur
- Can be utilized with other types of treatment
Chemotherapy
Drug treatment that addresses cancers that have or can spread to other areas (See Chemotherapy for Metastatic Melanoma)
- Works to inhibit cancer cell growth
- Used effectively for some subtypes of sarcoma
- Can be given orally, intravenously, or in other ways
- Doses are carefully selected to target the specific type and stage of the cancer
- Can be utilized with other types of treatment
Targeting Therapy (Precision Medicine)
Drug treatments that seek very particular proteins or enzymes within cancer cells(See Melanoma Targeted Therapy)
- Inhibits cancer cell replication and growth
- Targets specific genes and proteins
- Can mark cancer cells so that they can be destroyed by the immune system
- Can prevent new blood vessels from forming that can boost tumor growth
- Can be utilized with other types of treatment
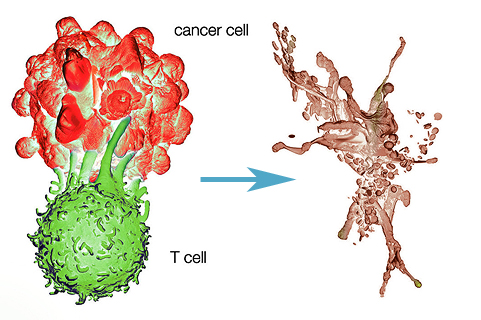
Immunotherapy
Helps to fight cancers by helping the body defend itself (See What is Immunotherapy for Cancer?)
- Effective against many kinds of cancers
- Supports conditions where cancer has spread throughout the body
- Blocks proteins that prevent an effective immune response
- Given intravenously over a period of weeks
- Can be utilized with other types of treatment
If you have questions regarding melanoma skin cancer or would like an expert second opinion, please call today or click here to schedule an appointment.