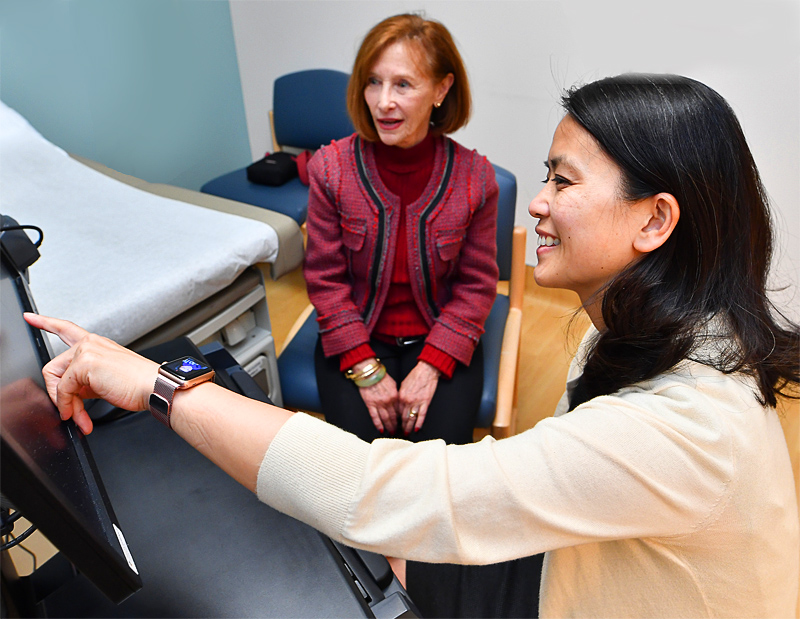
The Margie Petersen Breast Center at Providence Saint John’s Health Center is renowned for its comprehensive, multidisciplinary approach to breast care, offering a wide range of services to address various breast conditions. With a team of experts spanning multiple disciplines, our breast health center provides personalized care tailored to each patient’s needs.
We emphasize a patient-centered approach, prioritizing compassion, communication, and collaboration throughout the care journey. Integrated services provide seamless access to additional medical specialties and support services, such as genetics and nutrition. Proudly, our breast center has the ability to fully evaluate any breast problem in one day.
What is Breast Health?
Breast health encompasses a range of preventive measures, medical screenings, and oncologic care aimed at maintaining the well-being of breast tissue and addressing any potential issues, particularly breast cancer. Education plays a pivotal role in breast health, empowering individuals with knowledge about breast conditions they may be experiencing, self-examination techniques, and risk factors associated with breast diseases. Understanding the importance of regular screenings and early detection further enhances awareness and promotes proactive healthcare. Most conditions are not cancer, yet any breast-related concerns can be upsetting. We are here to help and guide you through the entire process.
Breast Evaluation
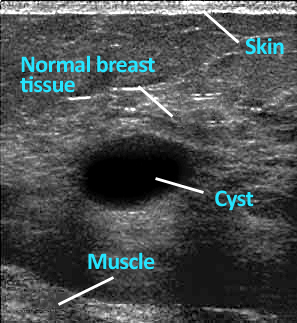
Screening is a cornerstone of breast health services, typically involving mammography, clinical breast exams, and in some cases, additional imaging modalities such as ultrasound or a brest MRI. Our imaging center aids in the early detection of breast abnormalities, potentially identifying cancerous or precancerous lesions at a stage when treatment is most effective. Regular screenings are particularly crucial for individuals with known risk factors, including age, family history, genetic predisposition (such as BRCA mutations), hormonal factors, and lifestyle habits like alcohol consumption and obesity.
Common Breast Evaluation Methods:

Screening tests
Mammograms are given routinely for patients who appear to be healthy and are not suspected of having breast cancer. The purpose of a mammogram is to find breast cancer early well before any symptoms begin to develop, and the cancer may be easier to treat.
Diagnostic tests
Diagnostic tests are performed if you have a breast abnormality or an abnormal screening test result. These tests are used to determine the type of abnormality found, and whether or not breast cancer is present. Diagnostic tests also are also used to gather more information if cancer is diagnosed, to guide decisions about treatment.
Oncologic care encompasses the diagnosis, treatment, and management of breast cancer. Evaluation often begins with a biopsy to confirm the presence of cancerous cells and determine their specific characteristics, which informs treatment decisions. If a biopsy is needed, we facilitate it the same day or as soon as possible. Our team of breast specialists can then quickly determine the next steps.
Treatment plans may include one or more of surgery, chemotherapy, radiation therapy, targeted therapy, or hormone therapy, tailored to the individual’s unique circumstances, such as tumor type, stage, and overall health. Survivorship care, addressing physical, emotional, and psychosocial aspects, is also integral to oncologic care, ensuring holistic support throughout the cancer journey and beyond.
Learn more about Breast Evaluation.
Breast Conditions
Understanding breast conditions is crucial for maintaining breast health and promoting early detection and intervention when necessary. Breast lumps or masses are one of the most common concerns and can vary in nature from benign cysts or fibroadenomas to malignant tumors like breast cancer. Regular breast self-exams and clinical screenings can help detect these abnormalities, enabling timely evaluation and treatment. Breast pain, although often benign, can also warrant medical attention to rule out underlying causes such as hormonal changes, infection, or musculoskeletal issues. Similarly, breast skin conditions like rashes or infections may signal dermatologic issues or, in some cases, inflammatory breast cancer, necessitating prompt evaluation by a healthcare professional.
High-risk breast lesions, such as atypical ductal hyperplasia or lobular carcinoma in situ (early development), merit close monitoring and possibly additional interventions to reduce the risk of developing breast cancer. Nipple conditions like inversion, discharge, or eczema can indicate various underlying issues, including hormonal changes, infection, or, rarely, malignancy. Additionally, while breast conditions are often associated with women, it’s important to recognize that men can also experience breast-related concerns, including gynecomastia (enlarged breast tissue) or, more rarely, breast cancer.
Learn more about conditions and symptoms:
From screening and diagnostic imaging to surgical interventions, oncologic treatment, and survivorship support, we offer a continuum of care under one roof, fostering convenience, coordination, and continuity of care for patients and their families.
Breast Cancer Risk Factors
A risk factor is anything that may increase your chance of developing a disease. Many risk factors are things you can control, like smoking, but others may be genetic. Knowing your risk factors for any disease can help guide you in taking appropriate actions to reduce your risk, including changing behaviors, and being clinically monitored for the disease.
Unmodifiable Risk Factors

- Gender. Breast cancer occurs nearly 100 times more often in women than in men.
- Race or ethnicity. It has been noted that white women develop breast cancer slightly more often than African-American women. However, African-American women tend to die of breast cancer more often. This may be due to the fact that African-American women often develop a more aggressive type of tumor. The risk of developing breast cancer and dying from it is lower in Hispanic, Native American, and Asian women.
- Aging. Most breast cancer is diagnosed in women after age 55.
- Previous radiation therapy to the chest during adolescence. Patients who had radiation therapy to the chest for another type of cancer are at greater risk of developing breast cancer.
- Family history. Having a close relative, such as a mother or sister, with breast cancer increases one’s risk of developing breast cancer.
- Genetic factors. Only about 5-10% of all breast cancer is known to be associated with an inherited genetic mutation. The most common mutations are in BRCA1 and BRCA2. If someone inherits such a mutation, the risk of developing breast cancer is much higher than for the average man or woman.
- Benign breast disease. Women with certain benign (not cancerous) breast conditions (such as atypical ductal or lobular hyperplasia, or lobular carcinoma in situ) have an increased risk of developing breast cancer.
- Mammographically dense breast tissue. Breast tissue may look dense or fatty on a mammogram. Women with dense breast tissue are at slightly increased risk of developing breast cancer. Dense breast tissue also makes it more difficult to see changes on a mammogram.
- Tomosynthesis makes this easier.
- Diethylstilbestrol (DES) exposure. Women who took this drug while pregnant (to lower the chance of miscarriage), and their daughters born from that pregnancy are at slightly higher risk.
- Early menstrual periods. Women whose periods began early in life (before age 12) have a slightly higher risk of breast cancer.
- Late menopause. Women are at a slightly higher risk if they begin menopause later in life (after age 55).
Modifiable Risk Factors
- Getting to and maintaining a healthy weight.
- Staying physically active.
- Limiting or eliminating alcohol from your diet.
Cancer Prevention
Prevention strategies are essential components of breast health, aiming to reduce the risk of developing breast cancer and other breast-related conditions. Lifestyle modifications, such as maintaining a healthy weight, engaging in regular physical activity, limiting alcohol intake, and avoiding tobacco use, can significantly influence breast health outcomes. Additionally, some patients may benefit from chemoprevention agents or risk-reducing surgeries, particularly those with a strong familial or genetic predisposition to breast cancer.
Nutrition & Physical Activity Guidelines
The World Cancer Research Fund estimates that about 20% of all cancers diagnosed in the US are related to body fat, physical inactivity, excess alcohol consumption, and/or poor nutrition. The American Cancer Society Guidelines recommend achieving and maintaining a healthy weight throughout life. These patient guidelines are summarized as follows:
- Be as lean as possible throughout life without being underweight.
- Avoid excess weight gain at all ages. Losing even a small amount of weight has health benefits and is a good place to start for those who are overweight or obese.
- Get regular physical activity and limit your intake of high-calorie foods and drinks.
- Adults: Get at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity activity each week (or a combination of these), preferably spread throughout the week.
- Children: Get at least 1 hour of moderate or vigorous intensity activity each day, with vigorous activity on at least 3 days each week.
- Limit sedentary behavior such as sitting, lying down, watching television, and other forms of screen-based entertainment.
- Eat a healthy diet, with an emphasis on plant-based food.
- Limit how much-processed meat and red meat you eat.
- Eat at least 2 ½ cups of vegetables and fruits each day.
- Choose whole grains instead of refined grain products.
- If you drink alcohol, limit your intake. It is recommended you drink no more than 1 drink per day for women and 2 per day for men.
10 Tips for Cancer Prevention
See Cancer.org for additional information.
For most adults, experts consider a Body Mass Index (BMI) within the range of 18.5 to 24.9 to be healthy, a BMI between 25 and 29.9 to be overweight, and a BMI of 30 and over to be obese. Body Mass Index is a screening tool that calculates your height and weight to determine your risk for weight-related diseases.
Carcinogen Exposure
Substances and exposures that can lead to cancer are called carcinogens. California’s Proposition 65, also called the Safe Drinking Water and Toxic Enforcement Act, requires the state to publish a list of chemicals, at least once a year, that are “known to the State of California to cause cancer or reproductive toxicity.” For more information, a complete list can be found on the California Office of Environmental Health Hazard Assessment website here.
By combining clinical excellence with compassionate care, the Margie Petersen Breast Center exemplifies a model of excellence in breast health, serving as a beacon of hope and healing for patients facing breast-related health challenges in their lives.
Contact the Margie Petersen Breast Center

The Margie Petersen Breast Center at Providence Saint John’s Health Center is widely renowned for its outstanding and compassionate patient care, expert surgical and medical team, and ability to fully evaluate any breast condition in one day.
Meet Our Breast Health Experts
The Breast Health Clinic can be reached at (310) 582-7209. If you have questions regarding a new symptom or want to make an appointment for evaluation please call and a staff member will assist with navigating you in the right direction.
Frequently Asked Questions (FAQs)
What can I expect at a breast clinic?
At a breast clinic, healthcare professionals provide specialized care for patients. They conduct comprehensive breast exams, mammograms, and ultrasounds to detect abnormalities. The center offers biopsies if necessary, ensuring accurate diagnoses. Patients receive personalized consultations to discuss their health, treatment options, and preventive measures. Clinics also provide support services, such as counseling and follow-up care, to guide patients through their health journey. By focusing on early detection and effective treatment, breast clinics aim to improve patient outcomes and overall well-being.
How often should I have a mammogram?
Patients should have a mammogram annually starting at age 40, according to many health experts. However, the frequency may vary based on individual risk factors. Consulting with a healthcare provider at a breast care center helps determine the best schedule. For those with a family history of breast cancer or other risk factors, more frequent screenings might be necessary. Regular mammograms are crucial for early detection, improving treatment outcomes. Discussing personal health history with a provider ensures a tailored approach to breast health and optimal care.
How do I prepare for a breast clinic appointment?
To prepare for a breast clinic visit, patients should gather medical records and any previous imaging results. Wear a two-piece outfit for easier access during exams. Avoid using deodorants or lotions, as they can affect mammogram images. Bring a list of current medications and note any breast changes or concerns. Arrive early to complete necessary paperwork. At the health center, communicate openly with healthcare providers about your symptoms and family history. Following these steps ensures comprehensive care and helps the medical team provide the best possible health evaluation and recommendations.