At Saint John’s Health Center, our radiation therapy services are provided by Vasek Polak Radiation Oncology, which provides comprehensive, state-of-the-art radiotherapy services. As part of a multi-disciplinary approach to patient care and treating cancer, including surgeons, medical oncologists, and radiation oncologists, we work together to ensure the most effective treatment plans for each patient.
What is Radiation Therapy for Breast Cancer?
Radiation therapy, also called radiotherapy, is a cutting-edge medical technique designed to target and treat cancerous tumors in the breast and other parts of the body. Typically, radiation is used to treat areas of the breast that are close to the surgery site. This helps to ensure any remaining cancer cells within the margin of treatment are destroyed, thereby reducing the possibility of recurrence. While radiation therapy kills cancer cells by damaging their ability to reproduce, it can also affect normal cells, so treatment must be carefully planned and calculated. This process minimizes the impact on the healthy surrounding tissues and organs. Radiation remains a highly effective way to destroy cancerous tumors, providing additional options beyond surgery.
The Vasek Polak Radiation Oncology Department at Saint John’s Health Center offers our patients access to highly advanced radiation therapy technology combined with a highly experienced and compassionate team of technologists and support staff.
Learn more about radiation technologies, including the roles and responsibilities of the radiation oncology care team.
Common Types of Radiation Therapy for Breast Cancer
Radiation can be delivered from outside the body through specialized machines or by positioning radioactive sources inside the body near cancer cells. How radiation is delivered will depend on the type and stage of cancer. Our approach involves a multidisciplinary team that collaborates to determine the best treatment plan for each patient. They will provide you with information when additional treatment modalities are recommended, ensuring patients can ask questions and tailor their care.
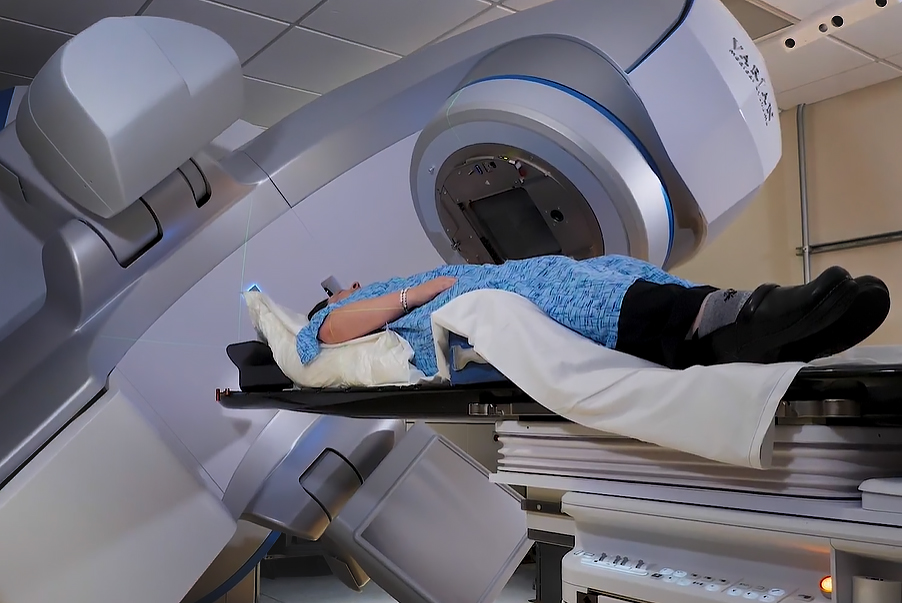
External Beam Radiation
The most common form of radiation therapy is external beam radiation, especially after procedures like lumpectomy or sometimes mastectomy. Our Varian Edge™ linear accelerator allows patients to receive precisely targeted higher-dose radiation in shorter, more comfortable sessions. This method is painless, and each session lasts just a few minutes. Before starting treatment, patients undergo a planning session, known as a simulation, which involves a CT scan to help our experts craft a personalized treatment plan that maximizes efficacy while minimizing impact on healthy tissues.
Intraoperative Radiation Therapy (IORT)
Intraoperative Radiation Therapy (IORT) is an innovative technique that administers radiation directly to the cancer site during surgery. This method is designed to maximize the protection of normal tissues while minimizing side effects. IORT is particularly beneficial because it delivers a high dose of radiation in a single session, immediately after the tumor is removed. This approach ensures that any remaining cancer cells are targeted effectively, reducing the likelihood of recurrence. The procedure involves placing a specialized applicator in the area where the tumor was removed, through which the radiation is delivered.
Despite its relatively recent introduction and shorter follow-up period, IORT has shown promising results in clinical trials. It is available to select patients based on specific criteria, such as tumor size and location, and overall health. In some cases, additional radiation therapy may be required after surgery to ensure comprehensive treatment. The integration of IORT into the surgical process involves close collaboration between the surgical and radiation oncology teams, ensuring that the treatment is both effective and safe. This multidisciplinary approach helps achieve excellent cancer control with minimal complications.
Accelerated Partial Breast Irradiation (APBI)
APBI offers another option for certain patients’ post-lumpectomy. This method targets the rim of normal tissue around the surgical site, allowing for a quicker treatment cycle compared to whole breast radiotherapy. Enveloping the site where the tumor was located, treatment is administered via a small balloon, or lumens device, as with SAVI, MammoSite, and Contura, which are commonly used for breast brachytherapy. APBI is typically administered twice daily over five days, using advanced technologies like Intensity Modulated Radiotherapy (IMRT) or High Dose Rate Brachytherapy (HDR).
While radiation therapy is generally well-tolerated, it’s normal to experience mild side effects, such as skin changes or fatigue, during the treatment course. Rest assured, our dedicated team—including your Margie Petersen Breast Center Nurse Navigator and radiation oncology nurses and physicians—will provide you with personalized care and detailed guidance throughout your journey.
Click here to learn more about radiation technologies.
Radiation after Lumpectomy or Mastectomy
Radiation therapy is a crucial component of breast cancer treatment, particularly following surgical interventions like lumpectomy or mastectomy. After a lumpectomy, radiation typically targets the remaining breast tissue to eliminate any residual cancer cells, significantly reducing the risk of recurrence. This approach, known as breast conservation therapy, often involves external beam radiation, which directs high-energy rays at the entire breast or, in some cases, just the area around the tumor site (partial-breast irradiation). The inclusion of nearby lymph nodes in the radiation field may be recommended if there is a risk of cancer spread.
In the case of a mastectomy, radiation therapy is generally considered when there are high-risk features such as large tumor size or lymph node involvement. The treatment focuses on the chest wall and adjacent lymph nodes to prevent recurrence in these areas. For patients who have undergone immediate breast reconstruction, a multidisciplinary team ensures that radiation therapy is seamlessly integrated into the treatment plan. This collaborative approach helps achieve excellent cancer control while minimizing radiation-related complications. Advances in radiation techniques, such as intensity-modulated radiation therapy (IMRT), have further improved the precision and effectiveness of post-mastectomy radiation, enhancing patient outcomes with fewer side effects.
At the Margie Petersen Breast Center, we are committed to supporting you every step of the way. For more information about radiation thereapy or other treatments, please contact our center.
Questions?
Contact the Margie Petersen Breast Center

The Margie Petersen Breast Center at Providence Saint John’s Health Center is widely renowned for its outstanding and compassionate patient care, expert surgical and medical team, and ability to evaluate any breast condition in one day fully.
Meet Our Breast Health Experts
The Breast Health Clinic can be reached at (310) 582-7209. If you have questions regarding a new symptom or want to make an appointment for evaluation please call and a staff member will assist with navigating you in the right direction.