The Margie Petersen Breast Center at Saint John’s Health Center is committed to offering comprehensive evaluation and screening services. Our goal is to provide peace of mind and help you understand the changes you may be experiencing. We aim to better understand the nature of your cancer, its genetics, your family history, and develop comprehensive treatment plans that are outcomes based.
About Breast Cancer
Breast cancer is one of the most common and well-known cancers diagnosed in the United States. It can occur in both women and men, but it is substantially more common in women. With increased awareness and support for breast cancer research, there have been many new advances in how breast cancer is treated. At the Margie Petersen Breast Center, we strive to bring you the most innovative care for your breast cancer and support for all of your breast health needs.
What are the Signs and Symptoms of Breast Cancer?
Knowing the signs and symptoms of breast cancer may help save your life. When the disease is discovered early, there are more treatment options and a better chance for a cure. Most painful breast lumps are not cancerous. Any discrete breast lump, whether painful or not, should be evaluated because breast cancer often presents as a lump or thickening.
Other potential signs of breast cancer include:
- Lump in the breast or in the underarm
- A spontaneous or bloody discharge from the nipple
- New retraction or indentation of the nipple
- A change in the size or contour of the breast
- Any flattening or indentation of the skin over the breast
- Redness or pitting of the skin over the breast, like the skin of an orange
- Crustiness, ulceration, or rash of the nipple or areola
- Swelling of all or part of a breast, even if no lump is felt
- Skin dimpling, sometimes resembling an orange peel
- Pain or tenderness in the breast or nipple
A number of conditions other than breast cancer can cause breasts to change in size or feel. Breast tissue changes naturally during pregnancy and a woman’s menstrual cycle. Other possible causes of non-cancerous (benign) breast changes include fibrocystic changes, cysts, fibroadenomas, infection, or injury.
If you find a lump or other change in your breast — even if a recent mammogram was normal — you should call us immediately. If you haven’t yet gone through menopause, you may want to wait through one menstrual cycle before seeing your doctor. If the change hasn’t gone away after a month, have it evaluated.
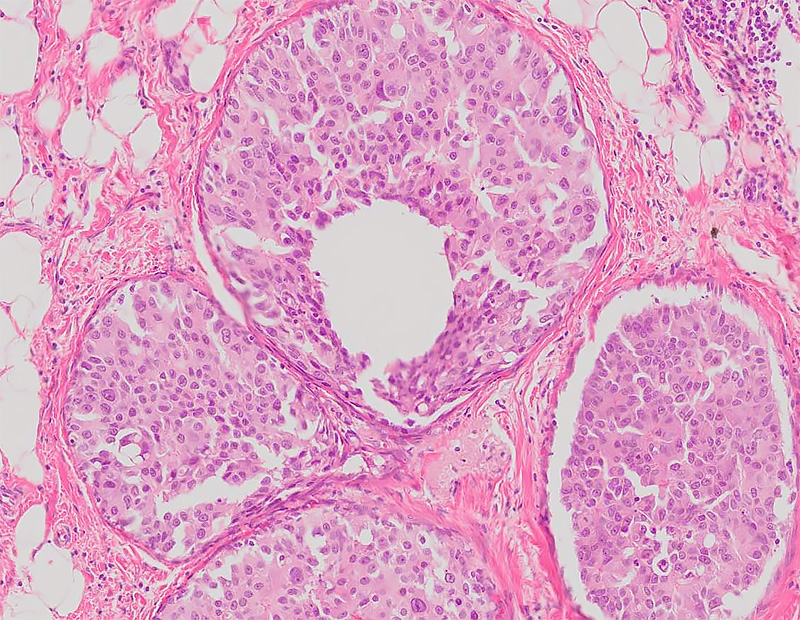
Pathology of Breast Cancer
What is a Histological Work-Up for Breast Cancer and why is it important?
A histological work-up for breast cancer is crucial because it provides a detailed microscopic analysis of the breast tissue, allowing pathologists to identify the presence and type of cancer cells. This evaluation helps determine the specific characteristics of the tumor, such as its size, grade, and stage, which are essential for accurate diagnosis and treatment planning. By examining the cellular and molecular properties of the tissue, pathologists can distinguish between benign and malignant lesions, ensuring that patients receive appropriate and timely interventions.
Moreover, histological analysis plays a vital role in guiding treatment decisions. It helps identify biomarkers that predict how a patient will respond to specific therapies, such as hormone treatments or chemotherapy2. For instance, immunohistochemical staining can detect proteins like HER2, which are important for targeted therapies in breast cancer3. This personalized approach to treatment improves patient outcomes by tailoring therapies to the unique characteristics of the tumor, ultimately enhancing the effectiveness of the treatment and reducing the risk of recurrence.
What is Histology?
Histology is the microscopic study of living tissues. There are four basic types of tissue in the body: epithelial tissue, muscle tissue, connective tissue, and nervous tissue. Breast cancer is a malignant transformation of epithelial tissue (usually glandular tissue). Fat (adipose) and fibrous tissue are both connective tissues, which may also form into suspicious lesions that show up on a mammogram. The exact nature of the suspected tumor can almost always be confirmed on histological evaluation.
When a suspicious breast lesion appears on your mammogram or ultrasound, a biopsy sample will likely be taken from the lesion and sent for histological evaluation by the pathologist. Various amounts of tissue may be required, so we may perform either a fine needle, core, or excisional biopsy, but generally, your Providence Saint John’s surgeon will try to remove as little tissue as possible while remaining confident that the sample is representative and taken from the right spot.
An initial biopsy sampling and analysis could be considered an extension of the breast cancer screening process, where breast cancer is either confirmed positive or confirmed negative. Once breast cancer is confirmed by the pathologist, the breast cancer staging process begins. At that time, an additional sampling of breast tissue may be required for more extensive histological evaluation, and the lymph nodes will also be sampled in some manner.
Histological Grade of Breast Cancer
What is the Histological Grade of Breast Cancer?
The histological grade of breast cancer is a measure of how much the cancer cells differ from normal breast cells. This grade helps predict the aggressiveness of the cancer and guides treatment options. Your Providence Saint John’s pathologist will determine the type of breast cancer and whether it is confined to the breast ducts (DCIS) or has reached infiltrative or invasive status. They will also assess if the cancer has metastasized to the lymph nodes in the axilla based on additional samples from that region.
How is the Histological Grade Determined?
The histological grade is determined by examining three key features of the cancer cells under a microscope:
- Tubule Formation: The degree to which the tumor cells form glandular structures.
- Nuclear Pleomorphism: The variability in the size and shape of the cell nuclei.
- Mitotic Count: The number of cells undergoing division.
Each feature is scored from 1 to 3, and the scores are added to give a final grade:
- Grade 1 (Well Differentiated): Lowest score, least aggressive.
- Grade 2 (Moderately Differentiated): Intermediate score, moderate aggressiveness.
- Grade 3 (Poorly Differentiated): Highest score, most aggressive.
The presence of necrosis (dead or dying cells) and calcifications may also be noted, as these can indicate a more aggressive cancer.
Immunohistochemical Markers
Immunohistochemistry (IHC) is used to detect specific proteins in cancer cells, providing valuable information about the cancer’s characteristics and potential response to treatment.
Estrogen and Progesterone Receptors
Breast cancers that express high levels of estrogen and progesterone receptors are likely to respond well to endocrine therapy. These receptors are detected in the nucleus of normal breast cells and many malignant cancer cells.
HER2: Human Epidermal Growth Factor Receptor 2
HER2-positive breast cancers tend to have a poorer prognosis but can be treated with targeted therapies like Trastuzumab and Pertuzumab, which have been shown to reduce recurrence and mortality rates.
Epidermal Growth Factor Receptor 1 (EGFR)
EGFR is associated with grade III breast tumors and is often accompanied by low levels of estrogen receptors and other poor prognostic features.
P53
Mutations in the P53 gene, which controls cell growth and death, can significantly increase the risk of death in breast cancer patients. This mutation is most commonly associated with tumors in premenopausal women.
BCL2
B-cell lymphoma 2 (BCL2) is an anti-apoptotic protein that can indicate a favorable prognosis for early-stage breast cancer.
Molecular Classification
Breast cancers can also be classified based on gene expression profiles into four main molecular subtypes:
- Luminal A: Hormone receptor-positive, excellent prognosis.
- Luminal B: Hormone receptor-positive, higher proliferation rates.
- HER2-enriched: HER2-positive, aggressive but treatable with targeted therapies.
- Basal-like: Triple-negative, most aggressive.
Markers of Breast Cancer Proliferation
Proliferation markers like Ki-67 are used to measure the growth rate of cancer cells. High levels of Ki-67 indicate rapid cell division and can predict the response to chemotherapy78. Other markers include p21, p27, cyclin E, and cyclin D189. However, it is still the presence of estrogen and progesterone receptors and Her2 that remain the most useful markers for determining the management of breast cancer.
Frequently Asked Questions
How does breast cancer start?
Breast cancer develops as a result a genetic change (mutation) that occurs in the breast cells which alters the function of those cells.
Can breast cancer be found early?
Regular breast cancer screening with mammogram is the best way to detect early breast cancer. Early detection not only improves survival but also provided patients with more options when it comes to treatment of their cancer.
What are the early signs of breast cancer?
Breast cancer is usually associated with any symptoms. Most patient who presents with cancer will not have noted any changes in their health. Some early signs that warrant work up for possible cancer include bloody nipple discharge, skin dimpling and or retraction of the nipple.
How quickly does breast cancer spread?
Not all breast cancers spread at the same rate. Some can be faster growing like the more aggressive types like triple negative breast cancer however most change or spread can take several months to several years.
What’s the worst breast cancer to get?
Triple negative breast cancer tends to be considered the worst type of breast cancer due to the tendency for rapid growth and limited treatment options. However, even within the triple negative breast cancer category there are different behaving cancers. It is best to discuss the diagnosis, treatment options and prognosis with your physician.
Do you feel unwell with breast cancer?
Most patients do not feel “unwell” when they have breast cancer. In fact the majority of patients do not feel any changes.
What is breast cancer pain like?
Breast cancer is rarely associated with pain.
Learn More
Contact the Margie Petersen Breast Center

The Margie Petersen Breast Center at Providence Saint John’s Health Center is widely renown for its outstanding and compassionate patient care, expert surgical and medical team, and ability to fully evaluate any breast condition in one day.
Meet Our Breast Health Experts
The Breast Health Clinic can be reached at (310) 582-7209. If you have questions regarding a new symptom or want to make an appointment for evaluation please call and a staff member will assist with navigating you in the right direction.