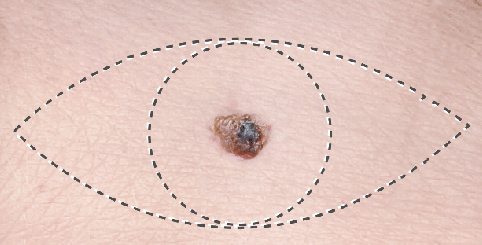
Our experience and research in melanoma are unmatched.
A History of Innovation and Collaboration
With the support of the Borstein Family Foundation, our melanoma program has maintained clinical excellence for more than 40 years, pioneering melanoma treatment under the leadership of the late Dr. Donald J. Morton—renowned cancer surgeon and melanoma researcher. Now as The Borstein Family Foundation Melanoma Program, the legacy endures.
Clinical trials at Saint John’s Cancer institute are multi-national, involving dozens of academic and industry organizations that work together to develop solutions and therapeutics. With highly advanced translational laboratories on site, our researchers and scientists can quickly identify patterns of cancer recurrence at the genetic and molecular level, which gives our clinicians greater insight to develop the most optimal treatment plans. Additionally, our immunology program works to understand how cancer cells evade treatment, which helps to promote targeted therapies specific to the biology of the patient.