What is Pancreatic Cancer?
Pancreatic tumors can’t be seen or felt by doctors during routine physical exams, and patients usually have no symptoms until cancer has spread to other organs, which is one of the main reasons why there are often poor outcomes for pancreatic cancer. Pancreatic cancer is the fourth most common cause of cancer death in the United States.
At the Saint John’s Cancer Institute in Santa Monica, CA, our gastrointestinal cancer surgeons diagnose and treat pancreas cancer with the most advanced therapies available.
We provide a multi-disciplinary approach to personalized care via a team of experts consisting of surgeons, medical and radiation oncologists, radiologists, gastroenterologists, pathologists, and specially trained support staff, all to help you make the most informed decision about your care.
About the Pancreas
The pancreas is a small gland located in the abdomen between the stomach and the intestines. It is mainly composed of the exocrine cells that make digestive enzymes and the endocrine (islet) cells that make hormones such as insulin, which controls blood sugar levels. Pancreatic cancer occurs when a cell in the pancreas is damaged and starts to grow out of control.
The vast majority of pancreatic cancers (adenocarcinoma) start in exocrine cells found in the pancreas ducts or small channels that carry digestive enzymes to the intestines. As pancreatic cancer grows, it can spread to surrounding organs – such as the bile duct, stomach, adjacent blood vessels, lymph nodes, and the liver.
Types of Pancreatic Cancer
The pancreas contains two main types of cells:
- Exocrine cells that produce digestive juices
- Endocrine cells that produce hormones
Adenocarcinoma
Starts in exocrine cells and accounts for 95 percent of pancreatic cancers. It occurs in the lining of the pancreatic ducts.
Islet cell carcinoma
Originates in the endocrine cells which make hormones such as insulin and glucagon. Most islet cell carcinomas are malignant, but insulin-producing islet cell tumors are often benign (non-cancerous). Islet cell tumors can be:
- Functional (produce high levels of hormones causing symptoms)
- Non-functional (produce no hormones) and symptoms are less obvious.
Pancreaticoblastoma
Is very rare. This type of pancreatic cancer is found mostly in young children. Isolated sarcomas and lymphomas can also occur in the pancreas. These are very rare.
Pseudopapillary neoplasms
Are mostly found in women in their teens and 20s. Patients can present with pain, jaundice (yellowing), weight loss, or a mass. These cancers mainly originate in the head of the pancreas. Resection of the tumor is often curative.
Ampullary cancer
Is a rare type of exocrine tumor that begins where the bile duct from the liver and the pancreatic duct joins with the small intestine. Since it causes jaundice and yellowing of the skin and eyes, it may be found earlier than other types of pancreatic cancer and therefore has a better outcome.
Rare Types of Pancreatic Cancer
Adenosquamous carcinoma and squamous cell carcinoma are rare types of pancreatic cancer.
Benign or Malignant Tumors
Insulinoma
Is a rare pancreatic tumor that secretes insulin, the hormone that lowers glucose levels in the blood.
Gastrinoma
Is a tumor that secretes above-average levels of gastrin, a hormone that stimulates the stomach to secrete acids and enzymes. Gastrinoma can also cause stomach ulcers and can spread to the liver.
Glucagonoma
Is a tumor that secretes glucagon, a hormone that raises levels of glucose in the blood, often leading to a characteristic rash.
Benign and pre-cancerous pancreatic lesions
Advances in imaging technology have dramatically increased the number of small abnormalities that are found in the pancreas. Most of these abnormalities are identified during imaging for another condition. Many of them are benign, fluid-filled cysts and are unlikely to cause symptoms or shorten a person’s life. Others are pre-cancerous and can develop into pancreatic cancer.
Can you screen for Pancreatic Cancer?
For many years, there were no preventive blood tests to find early cancers of the pancreas. Today, multi-cancer tests, such as Multi-cancer Early Detection (MCED) Testing, provides a measure for detecting more than 50 types of cancer in a single blood draw, including exocrine pancreatic cancer cells. Liquid biopsy tests are designed to identify biomarkers that are present for specific types of cancer.
The Carbohydrate Antigen (CA 19-9), which is released into the blood by exocrine pancreatic cancer cells, is the most extensively studied and validated serum biomarker for the diagnosis of pancreatic cancer in symptomatic patients. However, by the time CA 19-9 antigen levels are high enough to be detected, the cancer may no longer be in its early stages. This is why the CA 19-9 test is not recommended for routine screening of people without symptoms or for those who have a known history of cancer. The CA 19-9 test is sometimes used during treatment to see if the therapy is working or after treatment to see if the cancer has recurred.
Another substance, carcinoembryonic antigen (CEA), can help detect advanced pancreatic cancer in some people. But it isn’t sensitive enough to find the cancer early and is not recommended as a screening test.
How is Pancreas Cancer Diagnosed?
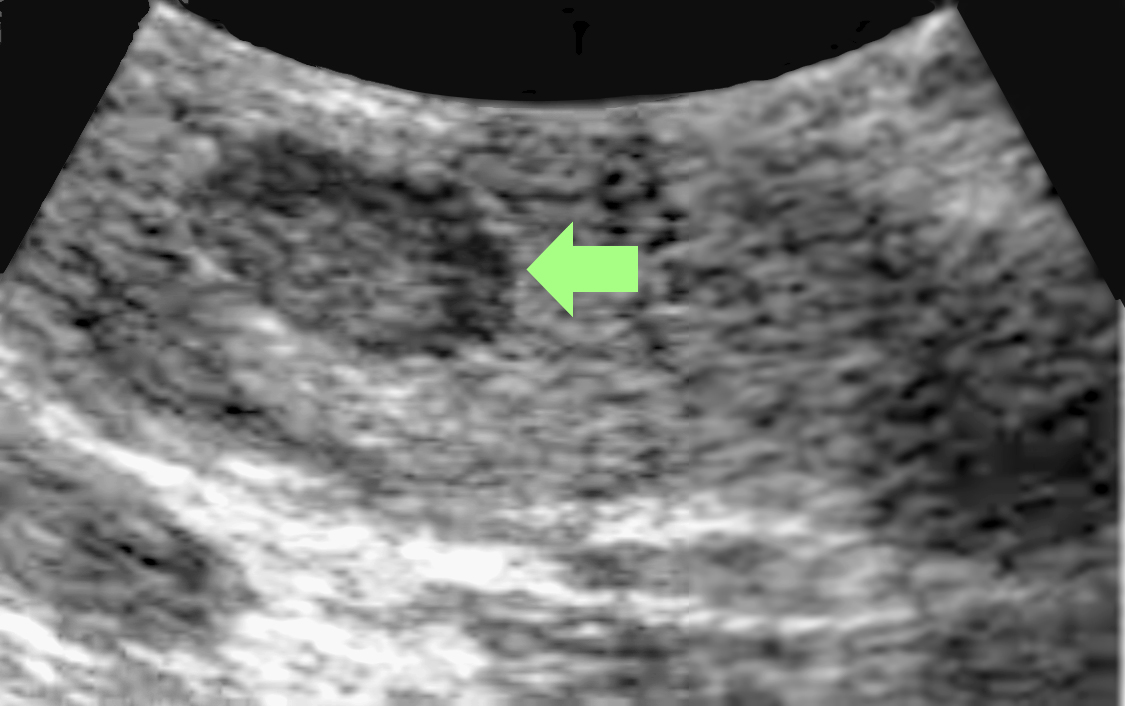
At Saint John’s Health Center and Cancer Institute, we take a complete medical history and do a physical exam before beginning any diagnostic procedures for pancreatic cancer. If pancreatic cancer is suspected, additional tests may be performed. Ultrasound (also called sonography) is a diagnostic imaging technique that uses high-frequency sound waves to create an image of the internal organs, specifically the liver, pancreas, spleen, and kidneys, and to assess blood flow through various vessels. The ultrasound may be done with either an external or internal device.
The images generated from ultrasound help us determine the size and location of a tumor in the pancreas and whether the tumor has spread to nearby blood vessels or other structures. Endoscopic ultrasound can also be used to obtain tissue samples. This is a type of biopsy called fine-needle aspiration. Cells obtained from the biopsy can then be analyzed more closely in a laboratory to see if they are cancerous.
Diagnosis Methods
Ultrasound
- Endoscopic ultrasound (EUS) is a procedure used to image the digestive tract, including the pancreas. A thin, flexible, lighted tube with a small ultrasound probe attached to the end is passed through the patient’s mouth into the stomach and the top part of the small intestine called the duodenum. The ultrasound component of the endoscope uses sound waves to create visual images of the pancreas.
- Transabdominal ultrasound involves placing an ultrasound device on the abdomen to create an image of the pancreas.
Genetic testing
Inherited DNA changes are thought to cause as many as 10 percent of pancreatic cancers. Because these inherited cases are sometimes linked with other cancers, determining whether a patient’s relatives have an increased risk is not simple.
Computed tomography scan (CT or CAT scan)
This diagnostic imaging procedure uses a combination of X-rays and computer technology to produce horizontal, or axial, images of the body. A CT scan shows detailed images of any part of the body including the bones, muscles, fat, and organs. CT scans are more detailed than X-rays and are the most important test to look for pancreas cancer and evaluate whether it can be removed surgically, or whether it has spread to other organs such as the liver or lungs.
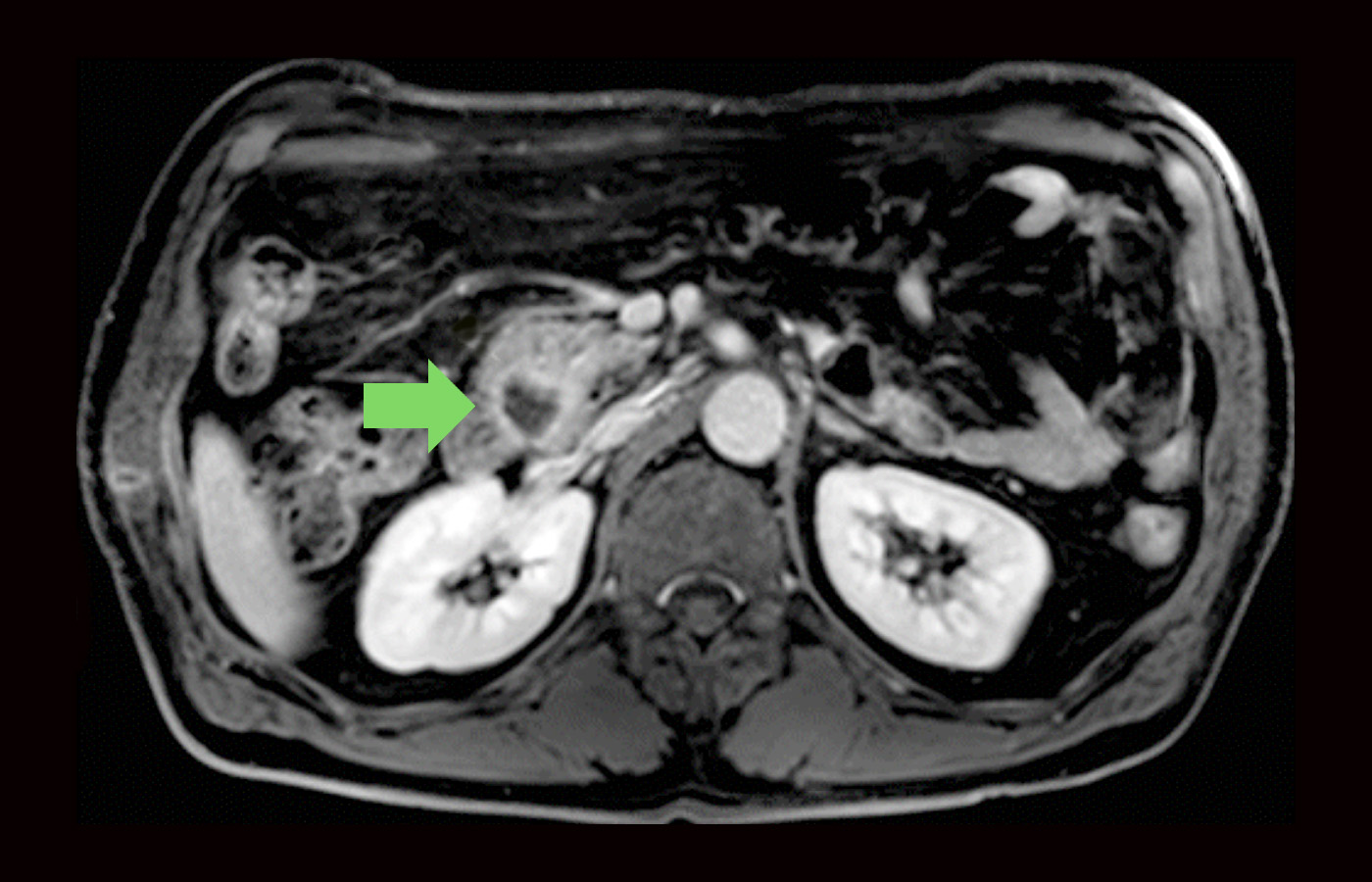
Magnetic resonance imaging (MRI)
An MRI is a diagnostic procedure that uses a combination of large magnets, radio frequencies, and a computer to produce detailed images of organs and structures within the body. Specific MRI evaluation of the bile duct, pancreas, and pancreatic duct is called magnetic resonance cholangiopancreatography (MRCP).
Endoscopic Retrograde Cholangiopancreatography (ERCP)
ERCP allows us to diagnose and treat problems in the liver, gallbladder, bile ducts, and pancreas. A long, flexible, lighted tube called an endoscope is guided through the mouth and throat, then through the esophagus, stomach, and duodenum (the first part of the small intestine). Providence Saint John’s physicians can examine the inside of these organs and detect any abnormalities. A tube is passed through the scope, and a dye is injected to allow the bile and pancreatic ducts to be seen on an X-ray.
Percutaneous Transhepatic Cholangiography (PTC)
During a PTC test, a needle is inserted through the skin and into the bile ducts. Dye (contrast) is injected through a needle which allows the small bile duct structures to be seen via X-ray. This test is generally only done if an ERCP cannot be done.
Pancreas biopsy
A sample of pancreatic tissue is removed with a needle or during surgery and then examined under a microscope.
Positron Emission Tomography (PET)
This is a type of nuclear medicine procedure. For this test, a radioactive substance, usually bound to a type of sugar, is injected through a vein before the body is scanned. The radioactive sugar collects in cancer cells, which will show up on images. This test is not as specific as CT scanning and is not used alone to diagnose pancreatic cancer. A PET scan is often done in combination with a CT scan and may be useful in evaluating whether cancer has spread to other organs such as the liver or lung.
Pancreatic Cancer Stages
Staging is a way of describing where the cancer is located, whether it has spread, and if it is affecting the functions of other organs in the body. Diagnostic tests including pathology are used to determine the stage, which is important to select the most appropriate treatment.
Stage 0
Refers to cancer in situ (situated in its place of origin), in which the cancer has not yet invaded outside the duct, or tube, in which it started (Tis, N0, M0).
Stage 1A
The tumor is 2 cm or smaller in the pancreas. It has not spread to lymph nodes or other parts of the body (T1, N0, M0).
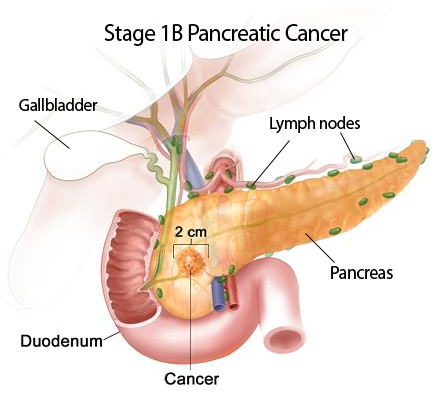
Stage 1B
A tumor larger than 2 cm is in the pancreas. It has not spread to lymph nodes or other parts of the body (T2, N0, M0).
Stage 2A
A tumor extends beyond the pancreas, but the tumor has not spread to nearby arteries or veins. It has not spread to any lymph nodes or other parts of the body (T3, N0, M0).
Stage 2B
A tumor of any size that has not spread to nearby arteries or veins. It has spread to lymph nodes but not to other parts of the body (T1, T2, or T3; N1; M0).
Stage 3
A tumor has spread to nearby arteries, veins, and/or lymph nodes but has not spread to other parts of the body (T4, N1, M0).
Stage 4
Any tumor that has spread to other parts of the body (any T, any N, M1).
Recurrent
Recurrent cancer is the return of cancer after treatment. If there is a recurrence, the cancer may need to be staged again (re-staging) using the system above.
Risk Factors for Pancreatic Cancer
Gender
More men than women are diagnosed with pancreatic cancer.

Age
Although pancreas cancer can occur in younger patients most occur in people over the age of 60.
Chronic pancreatitis
Chronic pancreatitis is long-term inflammation of the pancreas, often caused by excessive alcohol abuse, which has been linked to an increased risk for pancreatic cancer.
Smoking
Heavy cigarette smokers are two or three times more likely than nonsmokers to develop pancreatic cancer.
Obesity
Pancreatic cancer is more common in overweight, inactive people.
Diabetes
Pancreatic cancer occurs more often in diabetic patients.
Race
African-Americans are more likely than others to be diagnosed with pancreatic cancer and present with more advanced disease.
Workplace and Chemical Exposures
Exposure to certain occupational carcinogens like pesticides and chemicals used in the metal industry may increase the risk of pancreatic cancer.
Genetic factors
Most pancreatic cancer is not hereditary. A small percentage of patients have a familial type which can be associated with genetic mutations that are associated with melanoma or breast cancer. Mutations in the genes BRCA1 and BRCA2, which increase the risk of breast, prostate, and certain gynecologic cancers, have been found in some families with a history of pancreatic cancer.
Family History
The risk for developing pancreatic cancer is higher if a person’s mother, father, or sibling had the disease. An estimated 5 to 10 percent of people with pancreatic cancer have one or more family members who have had the disease. According to the National Cancer Institute, people with a strong family history of pancreatic cancer are nine times more likely to develop pancreatic cancer than others. Unfortunately, symptoms are often not known until the cancer is more advanced.

Non-specific symptoms include:
- Unexplained loss of appetite and weight loss
- Pain in the upper abdomen (belly) or upper back
- Jaundice (yellow skin and eyes, and dark urine)
- Indigestion, nausea, and vomiting can occur
- Extreme fatigue that does not improve
- Pale stools with or without dark urine
Other signs of pancreatic cancer may be found by a physician during an exam, even if there are no other noticeable symptoms. For example, an enlarged gallbladder or the sudden onset of type 2 diabetes may be indicators.
Pancreatic Cancer Treatment Summary
Depending on the type and stage, pancreas cancer may be treated in a variety of ways. Several factors are considered in planning your treatment. They include age, overall health, and medical history, as well as the type and location of the cancer.
Surgery
Surgery remains the most effective treatment for pancreatic cancer. It may involve the removal of the tumor, a section of the pancreas, or occasionally the entire pancreas. The type of surgery performed depends on the stage of pancreatic cancer, the location and size of the tumor, and your overall health. Types of surgery for pancreatic cancer include Whipple procedure, Distal pancreatectomy, Total pancreatectomy, and Palliative surgery.

Radiation
Since radiation is used to kill cancer cells and shrink tumors, special shields may be used to protect the tissue surrounding the treatment area. Radiation treatments are painless.
Chemotherapy
Chemotherapy involves the use of anticancer drugs to kill cancer cells. In most cases, chemotherapy works by interfering with the cancer cell’s ability to grow or reproduce.
Medication
Medication may be prescribed to help relieve or reduce pain as part of the treatment.
Learn more
Click here for Pancreatic Cancer Treatment.
Call today to learn more about Pancreatic Cancer Diagnosis and Treatment. Our multi-disciplinary team is ready to support you.
If you have questions regarding Pancreatic Cancer and symptoms, please call today. Click here to request an appointment.