The fellowship-trained breast surgeons at Providence Saint John’s Health Center offer the most advanced surgical breast techniques available, including oncoplastic lumpectomy/partial mastectomy surgery, extreme oncoplastic surgery, sentinel node biopsy, and skin-sparing and nipple-sparing mastectomy with breast reconstruction. At the Margie Peteresent Breast Center, we offer a comprehensive approach, involving many specialists collaborating on how to optimize treatment plans for each patient.
Breast-Conserving Surgery (Lumpectomy or Partial Mastectomy)
Breast-conserving surgery, also known as lumpectomy or partial mastectomy, aims to preserve as much of the breast tissue as possible. This is an effective option for patients with early-stage breast cancer. In this procedure, only the cancerous breast tissue, along with a small area of normal tissue surrounding it, is removed. While this is often preferable, breast-conserving surgery is not possible for all situations and is generally followed by radiation therapy. It’s important to understand that breast-conserving surgery has been shown to be just as effective as mastectomy in terms of survival. This surgery is usually performed as an outpatient procedure under mild sedation (a light form of anesthesia).
Whether or not you can undergo breast-conserving surgery depends on many factors, including the size of the cancer, the size of your breast, the number of cancer sites within the breast, and whether you can undergo subsequent radiation treatments. Incisions are often small enough to be hidden, and once healed, may even be difficult to see. With breast-conserving surgery, the nipple is almost always left in place. Our approach involves techniques that are least invasive, offering the best recovery and patient outcomes, and the most optimal post-surgical apearance of the breast.
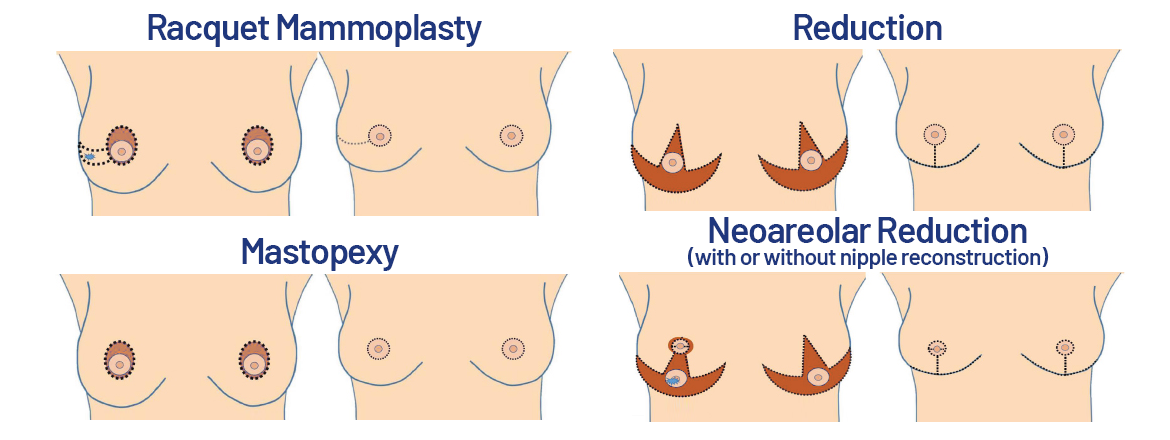
Oncoplastic Surgery
Oncoplastic surgery is a different approach to breast-conserving surgery. Specially trained breast surgeons use traditional plastic surgery incisions and techniques to perform the partial mastectomy. The benefit of oncoplastic surgery is to allow for wider removal of cancer with immediate reshaping of the breast tissue to provide an optimal cosmetic result. This approach has been shown to reduce the need for multiple operations to completely remove the cancer and is useful for removing larger cancers in patients who may otherwise have been advised to have a mastectomy. Oncoplastic surgery a good option for patients who are also candidates for breast reduction or mastopexy (breast lift). The opposite breast may also be modified to create symmetry.
Mastectomy
Mastectomy is a type of surgery that removes most of the breast tissue. Breast tissue extends from just below the collarbone to the fold under the breast, and from the breastbone to the side of the chest wall. When a mastectomy is performed, every effort is made to remove as much breast tissue as possible. However, there will be some residual breast tissue left under the skin. Mastectomy does not eliminate the risk of future breast cancer but will significantly reduce the risk to 1-3%. Radiation therapy can often be avoided in patients who have a mastectomy, although some patients with more advanced disease may still need radiation therapy afterward.
Types of Mastectomies
Total Mastectomy: During this surgery, the entire breast, nipple, and some skin are removed. This surgery is performed when the area of cancer is too large for breast-conserving surgery or for patients who cannot or will not have radiation therapy, or for men with breast cancer. This is usually done when patients are not interested in immediate reconstruction. Skin is removed so the patient is not left with excess skin after surgery. Breast reconstruction can still be done later to restore the appearance of the breast mound.
Skin-Sparing Mastectomy
This procedure removes the underlying breast tissue and nipple while preserving as much breast skin as possible. This leaves the breast skin envelope so that breast reconstruction can be performed with a better cosmetic result. This is always performed as part of a plan for reconstruction by the plastic surgeon.
Nipple-Sparing Mastectomy
This operation removes the entire breast but preserves the skin envelope and the nipple to maintain the appearance of the breast. The breast tissue is removed, but the overlying skin, nipple, and areola are left in place. An advantage of this procedure is that the breast remains more cosmetically attractive. The disadvantage is that the nipple and areola usually lose sensation.
Modified Radical Mastectomy
This is a total mastectomy with axillary lymph node dissection. During this procedure, the entire breast and the lower-level underarm lymph nodes are removed. The chest muscle is left intact. Breast reconstruction may be done by a plastic surgeon at the time of surgery or in the future to restore the appearance of the breast.
Oncoplastic Breast Surgery – A Novel Approach to Breast Cancer Surgery Webinar
Learn more about Oncoplastic Breast Surgery.
Breast Reconstruction
Breast reconstruction is a surgical procedure that rebuilds the breast contour after a mastectomy or lumpectomy. This process aims to restore the shape, appearance, and size of the breast, helping patients regain their confidence and sense of normalcy. There are two main types of surgical procedures to recreate the breast mound: using an implant or using your own tissue (also known as autologous reconstruction). Each method has its own benefits and considerations, and the choice depends on a patient’s unique situation, preferences, and medical history.
Using an implant involves placing a silicone or saline-filled prosthesis under the chest muscle or skin to recreate the breast shape. This method is often less invasive than using your own tissue and typically involves a shorter recovery time. Implants can provide a natural look and feel, and advancements in implant technology have improved their safety and durability. However, patients may need additional surgeries in the future to replace or adjust the implants.
Using your own tissue, also known as autologous reconstruction, involves taking tissue from another part of your body, such as the abdomen, back, or thighs, to create the new breast mound. This method can provide a more natural look and feel since it uses your own skin, fat, and sometimes muscle. Autologous reconstruction can be a more complex procedure with a longer recovery time, but it often results in a more permanent solution without the need for future surgeries to replace implants. In some cases, a combination of both methods may be used to achieve the desired volume and symmetry, offering the best of both worlds.
Lymph Node Surgery
For patients with invasive breast cancer, evaluating the lymph nodes in the armpit (axilla) is a critical component of the surgical procedure. Since breast cancer can spread through the lymphatic system, axillary lymph node surgery is the best way to determine if the cancer has spread beyond the breast.
Sentinel Lymph Node Biopsy
With this technique, usually only one or two lymph nodes are removed, making the surgery less invasive, with fewer complications, and allowing for a quicker recovery. This procedure can be performed along with either lumpectomy or mastectomy.
Axillary Lymph Node Dissection
This procedure is performed when there is biopsy-proven spread of cancer to the lymph nodes under the arm. A portion of fatty tissue under the arm containing lymph nodes is removed. The lymph nodes are separated from the fat and individually examined under the microscope by our pathologist. An average of 10 to 20 nodes are removed.
Lymphedema
One of the most significant complications of axillary lymph node dissection is lymphedema, or abnormal swelling of the arm or hand from impaired lymph drainage. It can develop immediately following surgery or even years later. Some patients also report swelling in the breast or chest wall. It may occur following the removal of some or all of the axillary lymph nodes or after radiation treatments directly to those nodes. It occurs when lymphatic vessels of the arm are no longer able to remove all the lymphatic fluid that is normally filtered from the tissue. Sometimes lymphedema is triggered by an injury, infection, burn, or other trauma to the arm. Studies have also shown that weight gain after treatment for breast cancer can strain the lymphatic system.
The Providence Saint John’s Health Center team of specialists includes physical therapists specially trained in treating lymphedema.
Frequently Asked Questions (FAQs)
What are the potential side effects of breast cancer surgery?
Understanding potential side effects can help you and your family prepare for recovery and the support services that follow. Patients can take a proactive role discussing any concerns with their healthcare team and plan for post-surgery care.
How long will it take to recover from breast cancer surgery?
Knowing the recovery timeline can help you and your loved ones plan accordingly. It also sets realistic expectations for the healing process and can help you arrange for any necessary support at home.
Will I need additional treatments after surgery?
It is important to understand the full scope of your treatment plan and who may be involved in your care. Knowing whether you will need radiation, chemotherapy, or hormone therapy after surgery can help you and your provider prepare for the next steps and any modifications of your cancer journey. We are ready to guide you every step of the way, providing educational materials and access to the specialists who have contributed to your treatment plan.
What are the options for breast reconstruction, and when can it be done?
Understanding reconstruction options helps patients make informed decisions about their post-surgery appearance and overall treatment plan. It also provides insight into the timing of reconstruction, whether it can be done immediately or at a later date.
How will breast cancer surgery affect my daily life and activities?
For most breast cancer patients, treatment is an out-patient procedure. However, there are practical aspects of recovery, such as physical limitations, pain management, and the impact on daily activities. Knowing the post-surgical effects can help you plan for any adjustments you may need to make in your daily routine and seek appropriate support.
We welcome your questions and hope that you reach out to us. Our gaol is to guide you through this process, whether a routine annual screening or more prolongued care. We are ready to support you.
Questions?
Contact the Margie Petersen Breast Center

The Margie Petersen Breast Center at Providence Saint John’s Health Center is widely renowned for its outstanding and compassionate patient care, expert surgical and medical team, and ability to evaluate any breast condition in one day fully.
Meet Our Breast Health Experts
The Breast Health Clinic can be reached at (310) 582-7209. If you have questions regarding a new symptom or want to make an appointment for evaluation please call and a staff member will assist with navigating you in the right direction.