Understanding how to identify and manage Cushing’s Syndrome is crucial for effective treatment and management. At Saint John’s Health Center, we treat all thyroid and adrenal conditions, including thyroid cancer, benign thyroid nodules, hyperparathyroidism, and Cushing’s Syndrome.
What is Cushing’s Syndrome?
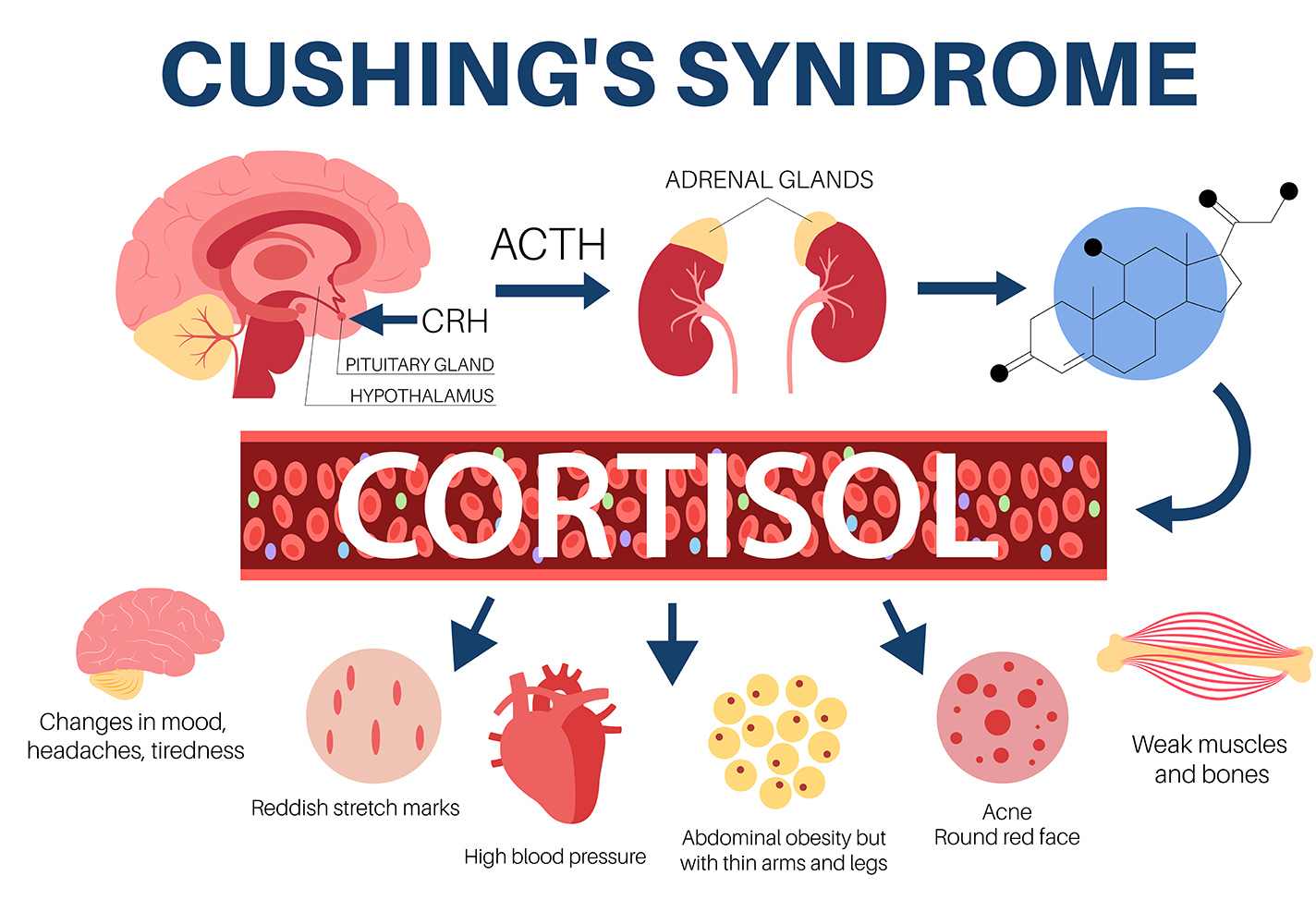
Cushing’s Syndrome is a medical condition characterized by prolonged exposure to high cortisol levels, a hormone produced by the adrenal glands. Cushing’s Syndrome is the term used when there is an abnormal, very high level of cortisol in the blood.This condition can result from various causes, including endogenous sources like tumors or exogenous factors such as prolonged steroid use. The primary causes of Cushing’s Syndrome include pituitary tumors, adrenal tumors, ectopic tumors, and excessive use of corticosteroids.
What are the signs and symptoms of Cushing Syndrome?
The signs and symptoms of Cushing’s Syndrome vary but often include notable physical changes and metabolic disturbances. Patients may experience fatigue and mid-section weight gain despite maintaining their usual diet and exercise routines. The redistribution of fat can lead to a rounded face, often referred to as a “moon face,” and a fatty hump between the shoulders. Bruising easily and swelling in the legs are common due to weakened blood vessels and fluid retention. Additional symptoms include high blood pressure and diabetes due to cortisol’s role in glucose metabolism and vascular tone regulation. Mood swings, depression, and cognitive impairments may also occur.
Some patients will present with little to no symptoms. However, lab results may indicate an underlying problem categorized as ‘subclinical Cushings’ and should still be considered for treatment.
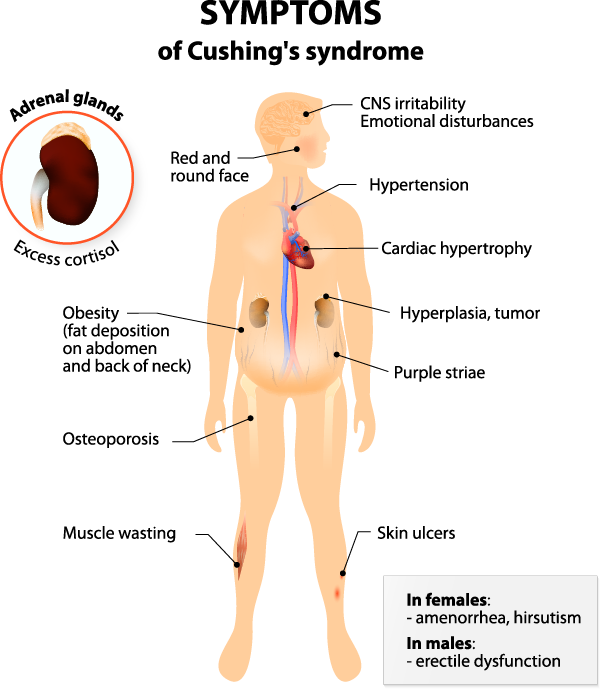
- High blood pressure
- Diabetes
- Moon facies (round facial shape)
- Buffalo hump (mound of fat at the back of the neck)
- Stretch marks
- Abnormal hair growth
- Osteoporosis
- Symptoms
- Easy bruising
- Fatigue
- Weight gain (particularly around the mid-section)
- Swelling in the legs
- Mood swings
- Irregular periods
- Muscle weakness
- Mental fogginess
There are 4 causes of Cushing syndrome. It is important to distinguish where the abnormal cortisol is coming from because the treatments are different based on the source.
Pituitary tumor
The most common cause (70-80%) of Cushing’s Syndrome is Cushing’s disease, which refers to tumors of the pituitary gland. Pituitary tumors result from benign tumors in the pituitary gland that secrete excessive amounts of adrenocorticotropic hormone (ACTH), stimulating cortisol production.
Adrenal tumor
Approximately 10% of patients with Cushing’s syndrome have an adrenal tumor, most commonly a benign adrenal nodule or bilateral adrenal hyperplasia that is producing excess cortisol directly. Adrenal cancer produces excess cortisol about 50% of the time, but it is a very rare tumor. Adrenal tumors directly increase cortisol levels, bypassing the regulatory control of ACTH.
Ectopic tumor
Approximately 10% of patients with Cushing’s syndrome have an ectopic cancer, most commonly in the lung, that produces cortisol or a similar and equivalent steroid hormone. Ectopic tumors, which can occur in the lungs, pancreas, or thymus, also produce ACTH, leading to high cortisol levels.
Use of excessive amounts of steroids
Steroids can also be a factor, creating the same symptoms and a pituitary or adrenal condition. Excessive steroid use for conditions like asthma, rheumatoid arthritis, or lupus can mimic the symptoms of Cushing’s Syndrome due to their cortisol-like effects.
Regardless of the cause, the symptoms are the same. However, many are either non-specific, common complaints or medical conditions and therefore the diagnosis is not always straight forward.
Risk Factors of Cushing’s Syndrome
Risk factors for developing Cushing’s Syndrome include chronic use of corticosteroid medications and predisposing genetic factors for tumors. Women are more likely than men to develop this syndrome, and it is most diagnosed in adults aged 30 to 50. Patients with conditions requiring long-term steroid therapy are at significant risk and should be monitored closely for signs of hypercortisolism.
There are a few hereditary endocrine tumor syndromes that increase one’s risk for pituitary and adrenal tumors, which can be cortisol producing, the most common being men. All patients with confirmed macronodular hyperplasia should be tested as well. If you have more than one hormone-producing tumor or multiple family members with these tumors, genetic testing and counseling is recommended.
How do you diagnose and treat Cushing’s Syndrome?
To diagnose Cushing’s Syndrome, healthcare providers rely on a combination of clinical evaluation, laboratory tests, and imaging studies. Initial screening tests include the 24-hour urinary free cortisol test, late-night salivary cortisol test, and the low-dose dexamethasone suppression test. Elevated cortisol levels from these tests indicate the need for further investigation. Imaging studies, such as MRI or CT scans, can identify tumors in the pituitary or adrenal glands. In some cases, petrosal sinus sampling may be necessary to distinguish between pituitary and ectopic sources of ACTH.
Diagnosis is made by a series of blood, salivary, and sometimes urine tests along with imaging (workup of adrenal tumors). These include not only your cortisol levels at specific times of the day but also deciphering where the source of the excess cortisol is coming from.
- Blood/urine tests to diagnose Cushing’s: salivary midnight cortisol, stimulated am cortisol
- Blood test to diagnose adrenal Cushing’s: ACTH (it will be low, or suppressed)
- Other blood/urine tests may be run to rule our other diagnoses that can have overlapping symptoms and for greater specificity.
- Certain medications can give a false positive result, so if your numbers are mildly elevated your physician may choose to repeat your labs and/or adjust your medications first.
- Imaging of adrenal Cushing’s: CT or MRI with contrast, adrenal protocol abdomen.
Once it is determined if the source is pituitary, adrenal, or an ectopic tumor, appropriate imaging (either a brain MRI or abdominal CT with special protocols) will be ordered.
Treatment and Management of Cushing Syndrome
Treatment for Cushing’s Syndrome depends on the underlying cause. Surgery is often the first-line treatment for tumors. For pituitary tumors, transsphenoidal surgery is typically performed to remove the tumor. Adrenal tumors may require adrenalectomy, while ectopic tumors necessitate surgical removal of the tumor producing ACTH. Medication is an alternative or adjunct to surgery, particularly if surgery is not feasible. Medications such as ketoconazole, mitotane, or metyrapone can inhibit cortisol production. For patients with endogenous Cushing’s Syndrome who are not surgical candidates, medications like mifepristone may help control symptoms.
In managing Cushing’s Syndrome, lifestyle modifications are also beneficial. Patients should maintain a balanced diet, engage in regular physical activity, and manage stress effectively. Regular follow-up with healthcare providers is crucial for monitoring cortisol levels and adjusting treatment plans as needed. Early diagnosis and tailored treatment strategies are essential for reducing complications and improving the quality of life for individuals with Cushing’s Syndrome.
Over time, many symptoms will resolve themselves. Weight loss, bruising, and a rounding face generally occur first. However, your body needs time to re-regulate itself, so these changes do not happen overnight. For instance, if you have newly diagnosed diabetes and/or high blood pressure that was caused by Cushing’s, they will likely improve over time and for a good number of patients, you will return to your pre-Cushing’s state. However, if conditions have been long-standing, there may be some lasting effects and therefore close monitoring by a medical professional is needed. Additionally, some autoimmune disorders may have been suppressed by the increased cortisol levels and so may appear/reappear after normalization of cortisol levels.
Prognosis and Follow-Up
After you have surgery for Cushing’s syndrome, you will meet with your surgeon two weeks after the operation. You will have regular appointments with your endocrinologist to monitor your blood tests and manage your medications. You will be slowly weaned off of steroids, a process that can take up to two years in some patients.
Many Cushing syndrome symptoms will go away after treatment, but this will most likely happen over time – up to 18 months. Weight loss, changing face shape, and reduced bruising are usually first. Additionally, if you have had long-standing issues caused by Cushing’s syndrome, there may be some long-term effects that require monitoring. Lastly, increased cortisol levels may have suppressed some autoimmune disorders. Once cortisol levels are normal, the disorders may come back.

If you have questions regarding thyroid cancer treatment or diagnosis, please call today. Click here to request an appointment.
Common questions you may want to ask your doctor about Cushing’s Syndrome
Q: What tests will you conduct to diagnose Cushing’s syndrome, and what should I expect during these tests?
Knowing the diagnostic process helps to prepare for the tests, understanding their purpose, and any potential discomfort. We typically start with a 24-hour urinary free cortisol test, a late-night salivary cortisol test, or a low-dose dexamethasone suppression test. These tests measure cortisol levels and help determine if your body is producing too much cortisol.
Q: What are the potential causes of my Cushing’s syndrome, and how will you determine the underlying cause in my case?
Identifying the cause is crucial for determining the appropriate treatment plan. Cushing’s syndrome can result from various factors, including medication use or tumors but can also be caused by long-term use of corticosteroid medications, adrenal tumors, pituitary tumors, or ectopic ACTH-producing tumors. Imaging tests like CT scans or MRI, along with blood tests, can be used to pinpoint the exact cause in your case.
Q: What treatment options are available for Cushing’s syndrome, and what are the potential side effects and success rates of each?
Understanding treatment options, their effectiveness, and potential side effects helps in making informed decisions about your care.
Treatment options include surgery, radiation therapy, medications to control cortisol production. Reducing corticosteroid use may also be recommended. Each treatment has its risks and benefits; for example, surgery has a high success rate but carries surgical risks, while medications can have side effects like fatigue and nausea.
Q: How will Cushing’s syndrome affect my long-term health, and what lifestyle changes or additional treatments might be necessary to manage the condition effectively?
Knowing the long-term impact helps in planning for ongoing management, necessary lifestyle adjustments, and understanding the prognosis. If left untreated, Cushing’s syndrome can lead to serious health issues like diabetes, osteoporosis, and cardiovascular problems. Managing the condition might involve lifestyle changes such as a healthy diet, regular exercise, and possibly ongoing medical treatments. We’ll also monitor your bone health, blood sugar levels, and cardiovascular health closely.





