Thyroid cancer is the most common cancer in women under 30 and the second most common cancer in women 30 to 45 years of age. At Saint John’s Health Center, we treat all thyroid and adrenal conditions including thyroid cancer, benign thyroid nodules, hyperparathyroidism, and Cushing’s Syndrome.
What is Thyroid Cancer?
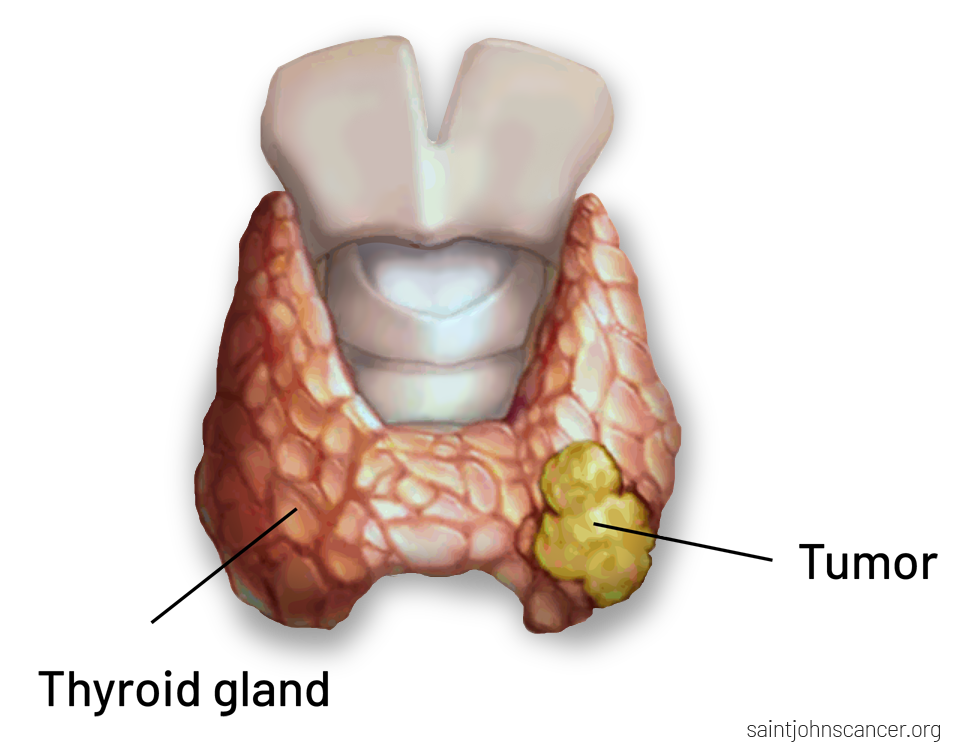
Thyroid cancer is a disease of the thyroid gland. It occurs when there is an abnormal, invasive growth of mutated thyroid cells. Thyroid cancer is usually very slow-growing, which means it mostly remains confined to the thyroid gland or extends no further than the surrounding lymph nodes. Most types of thyroid cancer are treatable and patients go on to live long, healthy, normal lives.
The only risk factors for thyroid cancer are a history of having received radiation to the head and neck or persons with a family history of an endocrine tumor syndrome, specifically Multiple Endocrine Neoplasia (MEN) type 2A and 2B. Thyroid cancer is rarely part of other cancer syndromes.
What are the symptoms of thyroid cancer?
Most thyroid cancers do not produce any symptoms. However, if large enough in size (and this is different for everyone), it may cause:
- Visible protrusion (lump or bump) in the neck
- Pressure in the front of the neck
- Difficulty or uncomfortable swallowing
- Problems breathing when lying flat
- A new persistent cough
- A change in your voice (though rarely)
- Changes in thyroid hormone production and endocrine balance in the body

How is Thyroid Cancer diagnosed?
All suspicious thyroid nodules should be evaluated by an expert using special ultrasound equipment, also scanning the lymph nodes near the thyroid gland. At that time, a biopsy may be recommended. Most types of thyroid cancer can be diagnosed with a biopsy, whereas some thyroid cancers may require surgical removal to reach a definitive diagnosis.
Thyroid cancer evaluation may include:
- Physical examination, observing your neck for nodules in the thyroid and reviewing your risk factors.
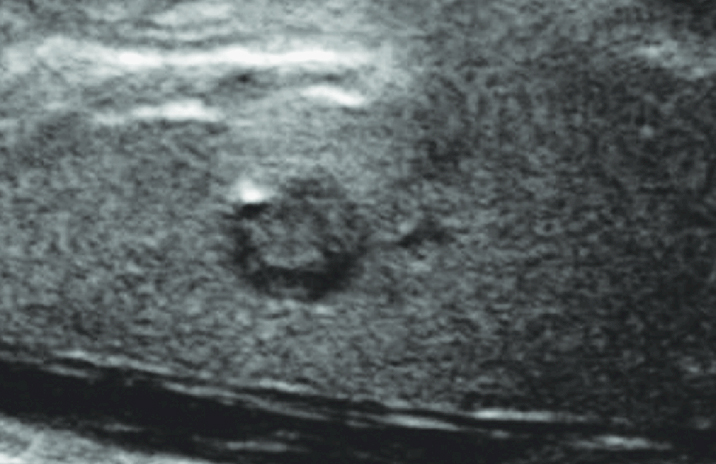
- Ultrasound imaging allows the doctor to generate visual images of the thyroid and surrounding tissues. This is the first step in identifying the likelihood of cancer. Additional tests would be needed to confirm a diagnosis and determine the type of thyroid cancer.
- Biopsy involves removing a sample of thyroid tissue. This is performed using a fine needle to remove some suspicious cells from the thyroid. At Saint John’s Health Center, we aim to provide analysis the same day as your biopsy.
- Radioactive tracing is an imaging method that uses radioactive iodine to detect thyroid cancer cells. It is primarily used after surgery to find any cancer cells that might remain and is most helpful for papillary and follicular thyroid cancers. Thyroid cancer cells absorb the iodine, which is revealed on the radioactive iodine scan images.
- CT scan of the neck is advised for more advanced thyroid cancers prior to surgery. This helps to verify the extent of tumor growth into the neck while supporting operative planning.
- Genetic testing is recommended for cases involving medullary thyroid cancer. Having an inherited gene can help us understand your risk of other types of cancer and your children.

Thyroid Cancer: Are you at Risk?
Dr. Melanie Goldfarb discusses thyroid cancer growth and spread.
Different Types of Thyroid Cancer
Papillary Thyroid Cancer (PTC)
The most common type of thyroid cancer, which accounts for 90-95% of cases, is papillary thyroid cancer. Papillary cancer is usually slow growing and can successfully be removed surgically. Though cancer can metastasize to the surrounding lymph nodes, this does not affect prognosis in most cases, and most patients do very well.
Follicular (FTC) and Hurthle cell thyroid cancer
FTC and Hurthle Cell thyroid cancer are two distinct types of cancer but are often discussed together and makeup 5 to 10% of all thyroid cancers. Follicular thyroid cancer spreads through the bloodstream to the lungs and bone, but not to the lymph nodes.
Hurthle Cell thyroid cancer can spread to lymph nodes or internal organs and is slightly more aggressive than papillary thyroid cancer. To diagnose these cancers, the nodule is removed and examined under a microscope by a pathologist.
Medullary Thyroid Cancer (MTC)
MTCs are a rarer form of thyroid cancer, accounting for 3 to 10% of all thyroid cancers. This type of cancer appears in patients with hereditary endocrine tumors and is more aggressive than PTC and FTC. Surgery is the only form of treatment for MTC, so a successful operation is critical. Due to the aggressive nature of MTCs, it is recommended that all patients have their thyroid removed (total thyroidectomy) as part of their treatment.
Anaplastic Thyroid Cancer (ATC)
ATCs account for about 1% of all thyroid cancers and are the most aggressive type of thyroid cancer. It usually occurs in older patients. Anaplastic thyroid cancer presents as a rapidly growing hardened mass in the neck, which tends to have a poor prognosis.
Premalignant’ or Self-contained Thyroid Cancer Types
Noninvasive Follicular Variant of Papillary Thyroid Cancer (NIFTP)
NIFTPs are a newer classification of thyroid cancer. These tumors also need to be removed surgically, but as cancer has not yet spread to surrounding tissues, a limited surgical approach is sufficient. This is achieved through thyroid lobectomy—surgery that involves removing about half of the thyroid gland including the portion of the thyroid that contains the suspicious tumor.
Minimally Invasive Follicular Thyroid Cancer (MIFTC)
MIFTCs are considered a contained follicular tumor, having only small to medium vessel invasion within or immediately adjacent to the tumor capsule without extending into the thyroid parenchyma. These tumors still need to be removed surgically. However, because the cancer has not yet spread, a limited surgical approach is recommended. This is achieved through thyroid lobectomy—surgery that involves removing about half of the thyroid gland including the portion of the thyroid that contains the suspicious tumor.
Thyroid Cancer Treatment
Historically, there were 3 components to thyroid cancer treatment: surgery, radioactive iodine, and thyroid hormone suppression. However, more recent thyroid cancer treatment has shifted toward a more conservative, minimally invasive approach, which is favored by most patients.
Active Surveillance
This strategy is being offered to select patients (mostly older) with small, 1cm (about 0.39 inches) or fewer tumors. Saint John’s has an active surveillance program and if you think you may be a candidate, we can discuss this option with you. Contact us to schedule an appointment.
Surgery
Most patients will need to undergo thyroid surgery to remove the thyroid cancer. The extent of your surgery (thyroid lobectomy vs total thyroidectomy) will depend on the size of your cancer, if the thyroid cancer extends beyond the thyroid gland, and if you have nodules in your other thyroid lobe.
Radioactive iodine
After a total thyroidectomy (removal of the thyroid gland), some intermediate to high-risk patients with more aggressive cancers may require additional treatment using radioactive iodine.
Thyroid hormone replacement
All thyroid cancer patients that have had their thyroid removed will be prescribed thyroid medication. Very high-risk patients will be given larger, suppressive doses of thyroid hormone replacement. This will help prevent any remaining thyroid tissue or cells from regrowing or returning in the form of cancer. Your Thyroid Stimulating Hormone (TSH) levels will be monitored by your endocrinologists to obtain your optimum dose.

If you have questions regarding thyroid cancer treatment, or diagnosis, please call today. Click here to request an appointment.
Common Thyroid Cancer Questions (FAQs)
Can my thyroid cancer come back after surgery?
Thyroid cancer can come back many years after your initial treatment, which is why it is particularly important to have regular checkups with your endocrinologist. They will perform scheduled ultrasounds to verify if there are changes since the prior scan.
If cancer comes back, it is usually in the thyroid bed where your thyroid was previously removed, or in the neighboring lymph nodes.
Are there risk factors for recurrence?
There are multiple staging systems for predicting recurrence in thyroid cancer that are each inclusive/exclusive of different prognostic factors. The most common one used today is the ATA Risk Stratification System which places patients in very-low, low, intermediate, or high-risk categories for recurrence.
Factors for recurrence include age, tumor size, lymph node involvement, distant metastases, histological subtype, histological features (invasion of the capsule, spread to the surrounding tissues, invasion of the lymphatics and blood vessels), and molecular tumor markers.