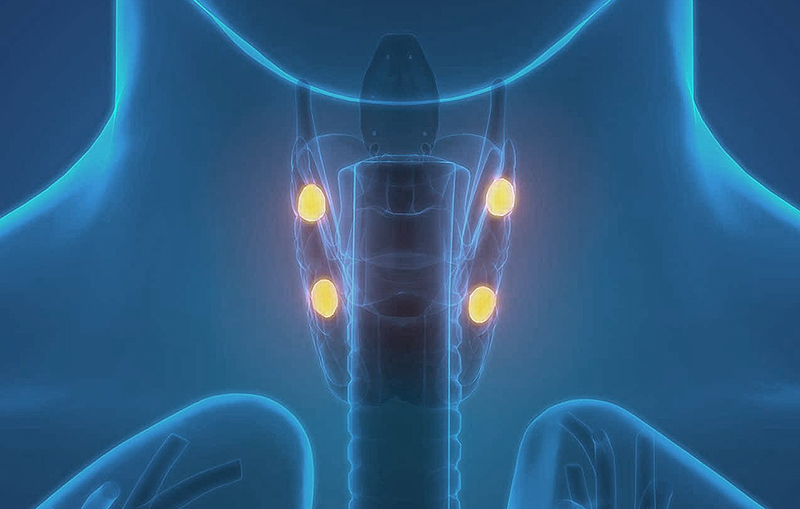
If you have questions regarding Parathyroid and Hyperthyroidism, please call today. Request an appointment
Melanie Goldfarb, M.D., M.Sc., FACS, FACE
Director, Center for Endocrine Tumors and Disorders
Medical Director for Cancer Survivorship
Dr. Melanie Goldfarb is a fellowship-trained endocrine surgeon and Director of the Center for Endocrine Tumors and Disorders. Her expertise is minimally invasive surgery for thyroid cancer and disorders, hyperparathyroidism, and adrenal tumors, including pheochromocytoma, Cushings, Conns, and adrenal cancer.