Thyroid cancer is the most common cancer in women under 30 and the second most common cancer in women 30 to 45 years of age. At Saint John’s Health Center, we treat all thyroid and adrenal conditions including thyroid cancer, benign thyroid nodules, hyperparathyroidism, and Cushing’s Syndrome.
What is Thyroid Cancer?
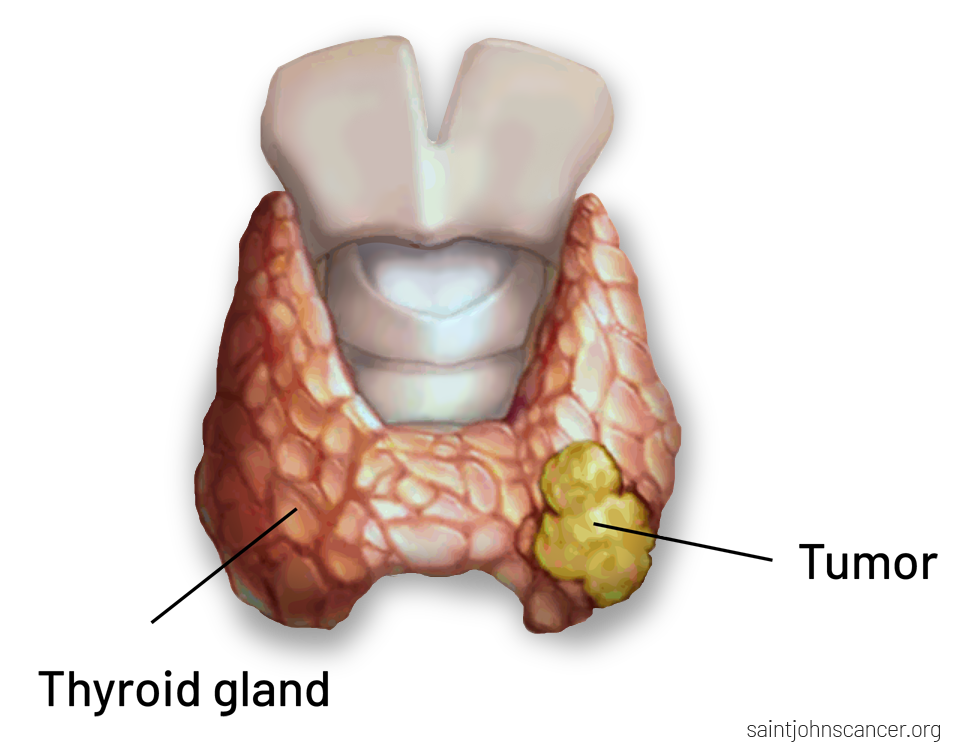
Thyroid cancer occurs when abnormal cells develop in the thyroid gland, forming nodules or tumors that may affect hormone production. Most thyroid cancers are highly treatable, especially when diagnosed early.
At Saint John’s Health Center in Santa Monica, our Endocrine Center of Excellence provides comprehensive thyroid cancer evaluation, ultrasound, biopsy, surgical management, and long-term follow-up led by a multidisciplinary team of thyroid specialists.
Understanding Thyroid Cancer
The thyroid gland, located at the base of the neck, produces hormones that regulate metabolism, heart function, and body temperature. Thyroid cancer often develops in thyroid nodules, which may be detected during routine exams or imaging studies.
Because many thyroid cancers grow slowly, early detection—through ultrasound and biopsy—is key to ensuring excellent outcomes.
Types of Thyroid Cancer
Thyroid cancer is not a single disease. There are several distinct types, each with different growth patterns, treatment approaches, and long-term outcomes. Identifying the specific type of thyroid cancer is an important first step in creating a personalized treatment plan.
Papillary Thyroid Cancer (Most Common)
Papillary thyroid cancer accounts for approximately 80% of all thyroid cancer cases. It typically grows slowly and often spreads to nearby lymph nodes in the neck. Despite this tendency to spread locally, papillary thyroid cancer has an excellent prognosis, especially when diagnosed early and treated appropriately. Most patients achieve long-term remission with surgery and, in some cases, additional therapy.
Follicular Thyroid Cancer
Follicular thyroid cancer is less common than papillary cancer and is more likely to spread through the bloodstream to areas such as the lungs or bones. When detected early, it is highly treatable and associated with excellent outcomes. Accurate diagnosis is essential, as treatment planning may differ slightly from other thyroid cancer types.
Medullary Thyroid Cancer (MTC)
Medullary thyroid cancer develops from C-cells in the thyroid, which produce the hormone calcitonin. This type of thyroid cancer may occur sporadically or as part of inherited syndromes, such as Multiple Endocrine Neoplasia type 2 (MEN2). Because of its genetic associations, diagnosis often includes specialized blood tests and genetic counseling to guide treatment and family screening.
Anaplastic Thyroid Cancer
Anaplastic thyroid cancer is rare but highly aggressive and fast-growing. It often presents with rapidly enlarging neck masses and symptoms affecting breathing or swallowing. Treatment typically requires immediate coordination among multiple specialists and may involve a combination of surgery, radiation therapy, chemotherapy, or targeted therapies when appropriate.
Understanding the cancer type guides treatment decisions, such as whether surgery alone is sufficient or additional therapies are needed.
Premalignant’ or Self-contained Thyroid Cancer Types
Noninvasive Follicular Variant of Papillary Thyroid Cancer (NIFTP)
NIFTPs are a newer classification of thyroid cancer. These tumors also need to be removed surgically, but as cancer has not yet spread to surrounding tissues, a limited surgical approach is sufficient. This is achieved through thyroid lobectomy—surgery that involves removing about half of the thyroid gland including the portion of the thyroid that contains the suspicious tumor.
Minimally Invasive Follicular Thyroid Cancer (MIFTC)
MIFTCs are considered a contained follicular tumor, having only small to medium vessel invasion within or immediately adjacent to the tumor capsule without extending into the thyroid parenchyma. These tumors still need to be removed surgically. However, because the cancer has not yet spread, a limited surgical approach is recommended. This is achieved through thyroid lobectomy—surgery that involves removing about half of the thyroid gland including the portion of the thyroid that contains the suspicious tumor.
Signs and Symptoms of Thyroid Cancer
Most thyroid cancers do not produce any symptoms. However, if large enough in size (and this is different for everyone), it may cause:
- A lump or swelling in the neck
- Voice changes or hoarseness
- Difficulty swallowing
- Neck pain or pressure
- Enlarged lymph nodes
- Persistent cough not related to illness
- Family history of thyroid cancer
- Genetic syndromes (MEN2, familial medullary thyroid cancer)
- Radiation exposure to the head, neck, or chest
- Female sex
- Personal history of thyroid nodules
- Iodine deficiency (rare in the U.S.)

Risk Factors for Thyroid Cancer
Genetic counseling may be recommended for patients with medullary thyroid cancer or a strong family history.
How is Thyroid Cancer diagnosed?
Diagnosing thyroid cancer involves a careful combination of clinical evaluation, imaging, tissue sampling, and laboratory testing. This comprehensive approach helps determine whether a thyroid nodule is cancerous, identifies the specific cancer type, and guides personalized treatment planning.
Physical Examination
Evaluation often begins with a physical exam of the neck to assess for thyroid nodules or enlarged lymph nodes. Your physician will also review personal and family medical history, radiation exposure, and other risk factors that may influence diagnosis and management.
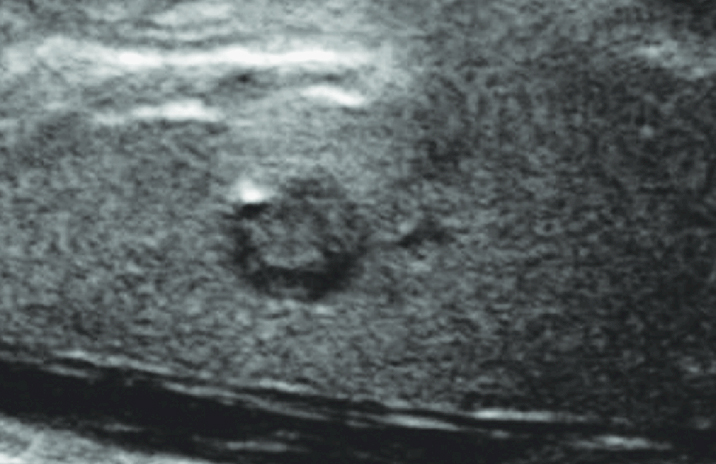
Thyroid Ultrasound
A thyroid ultrasound is typically the first imaging study performed when a nodule is detected. This noninvasive test evaluates the size, structure, and appearance of thyroid nodules and surrounding lymph nodes, helping determine whether further testing—such as biopsy—is needed.
Fine-Needle Aspiration (FNA) Biopsy
A fine-needle aspiration biopsy is the most reliable method for determining whether a thyroid nodule is benign or malignant. Using ultrasound guidance, a thin needle collects cells for microscopic analysis. At Providence Saint John’s Health Center, biopsy samples are evaluated promptly to support timely diagnosis and next-step planning.
Blood Tests
Blood testing helps assess thyroid function and identify tumor markers that may suggest specific cancer types. These tests may include thyroid-stimulating hormone (TSH), thyroid hormone levels, and—when medullary thyroid cancer is suspected—calcitonin and carcinoembryonic antigen (CEA) levels. These may include:
- Thyroid-stimulating hormone (TSH) and thyroid hormone levels to assess overall thyroid health
- Calcitonin and carcinoembryonic antigen (CEA) levels when medullary thyroid cancer is suspected
Blood test results help support diagnosis and may play a role in monitoring treatment response over time.
Additional Imaging
When thyroid cancer is advanced or there is concern for spread beyond the thyroid, additional imaging may be recommended. CT scans or MRI can help evaluate tumor extension into the neck and surrounding structures, supporting surgical planning. In select cases—often after surgery—radioactive iodine scanning may be used to detect remaining thyroid cancer cells, particularly in papillary and follicular thyroid cancers.
Genetic Testing
Genetic counseling and testing are recommended for patients with medullary thyroid cancer. Identifying an inherited mutation helps guide treatment decisions and provides important information for family members who may also be at risk.
Diagnosis of thyroid cancer integrates imaging, biopsy results, laboratory findings, and individual risk factors. This thorough approach ensures that treatment recommendations are precise, appropriate, and aligned with each patient’s condition and long-term health goals.
Staging Thyroid Cancer
Staging describes how far thyroid cancer has progressed and plays an important role in guiding treatment decisions and follow-up care. It helps determine whether the cancer is confined to the thyroid or has spread to nearby lymph nodes or distant organs.
Common factors used to determine thyroid cancer stage include:
- Tumor size and whether the cancer has grown beyond the thyroid gland
- Lymph node involvement, particularly in the neck
- Spread to distant sites, such as the lungs or bones
Staging allows the care team to tailor treatment—ranging from surgery alone to additional therapies—and to develop an appropriate long-term monitoring plan for each patient.
Thyroid Cancer: Are you at Risk?
Dr. Melanie Goldfarb discusses thyroid cancer growth and spread.
Thyroid Cancer Treatment
Historically, there were 3 components to thyroid cancer treatment: surgery, radioactive iodine, and thyroid hormone suppression. However, more recent thyroid cancer treatment has shifted toward a more conservative, minimally invasive approach, which is favored by most patients. Treatment for thyroid cancer is personalized based on the cancer type, stage, and individual patient factors such as age, overall health, and risk of recurrence. Your care team works closely with you to determine the most effective approach while preserving quality of life.
Thyroid Surgery (Primary Treatment)
Surgery is the main treatment for most thyroid cancers. Depending on the extent of disease, this may involve removing part of the thyroid (lobectomy) or the entire gland (total thyroidectomy). If cancer has spread to nearby lymph nodes, lymph node removal may also be performed to reduce the risk of recurrence and support accurate staging.
Radioactive Iodine (RAI) Therapy
Radioactive iodine therapy may be recommended after surgery for certain types of thyroid cancer, particularly papillary and follicular cancers. This treatment targets and destroys remaining thyroid tissue or microscopic cancer cells while limiting exposure to the rest of the body.
cThyroid Hormone Suppression Therapy
After surgery, patients often take thyroid hormone medication to replace normal hormone levels and suppress thyroid-stimulating hormone (TSH). Lowering TSH helps reduce the risk of cancer recurrence and supports long-term disease control.
Targeted Therapies & Immunotherapy
For advanced thyroid cancers or tumors that do not respond to radioactive iodine, targeted therapies or immunotherapy may be used. These treatments work by interfering with specific cancer pathways or enhancing the immune system’s ability to fight cancer.
External Beam Radiation or Chemotherapy
External beam radiation therapy or chemotherapy is typically reserved for aggressive or advanced thyroid cancers. These treatments may be used when surgery and radioactive iodine are not effective or as part of a combined treatment approach.

If you have questions regarding thyroid cancer treatment, or diagnosis, please call today. Click here to request an appointment.
Common Thyroid Cancer Questions (FAQs)
Can my thyroid cancer come back after surgery?
Thyroid cancer can come back many years after your initial treatment, which is why it is particularly important to have regular checkups with your endocrinologist. They will perform scheduled ultrasounds to verify if there are changes since the prior scan.
If cancer comes back, it is usually in the thyroid bed where your thyroid was previously removed, or in the neighboring lymph nodes.
Are there risk factors for recurrence?
There are multiple staging systems for predicting recurrence in thyroid cancer that are each inclusive/exclusive of different prognostic factors. The most common one used today is the ATA Risk Stratification System which places patients in very-low, low, intermediate, or high-risk categories for recurrence.
Factors for recurrence include age, tumor size, lymph node involvement, distant metastases, histological subtype, histological features (invasion of the capsule, spread to the surrounding tissues, invasion of the lymphatics and blood vessels), and molecular tumor markers.