If you have questions regarding Ureteral Cancer treatment, please call today. Click here to request an appointment.
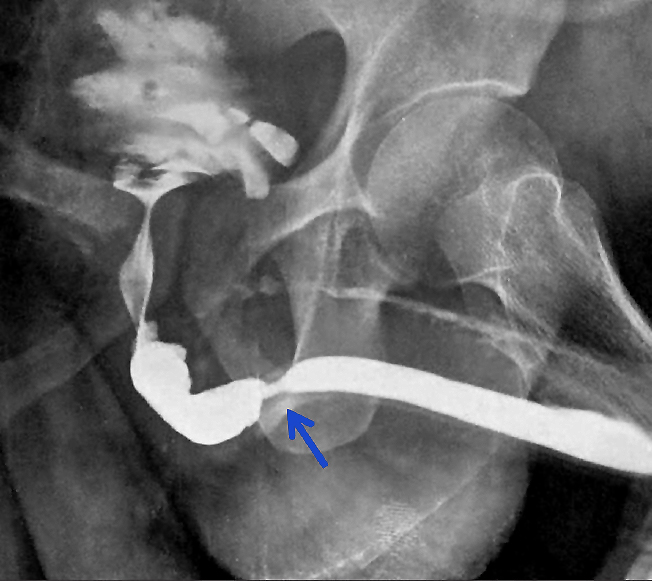
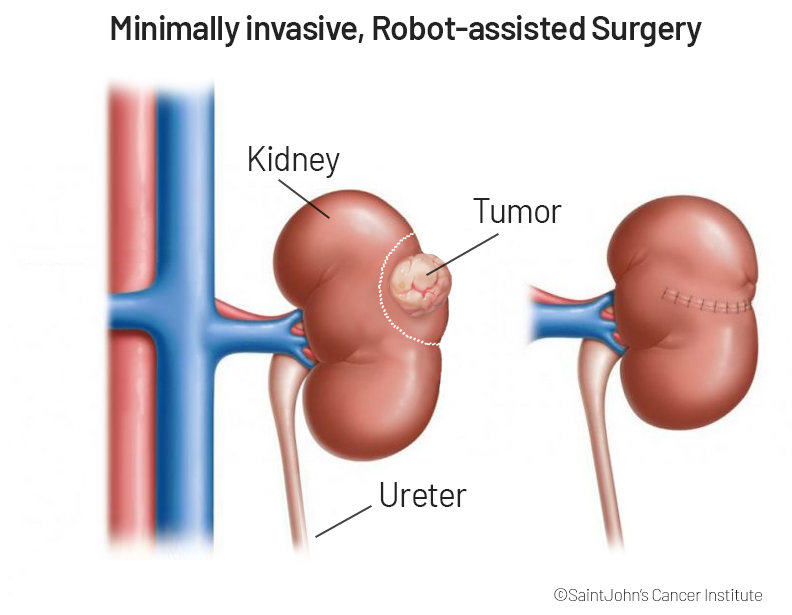
Ureteral Cancer and Upper Tract Urothelial Carcinoma (UTUC)
Ureteral Cancer and Upper Tract Urothelial Carcinoma (UTUC)
Schedule An Appointment
Saint John's: A Legacy of Care Excellence - 30 Major Healthcare Awards for 2022 and 2023 including Kidney Failure, Prostate Cancer Surgery, Surgical Care, and Uterine Cancer Surgery