Voiding Dysfunction requires a urology expert who can effectively determine the precise nature of the disorder. Our goal is to offer immediate and lasting relief, utilizing minimally invasive and best practice medical techniques.
What is Voiding Dysfunction?
Voiding dysfunction can encompass many disorders for many reasons including anatomical causes (structures of the body) as well as neurological causes (relating to the nervous system). This spans all the urinary conditions such as incontinence, overactive bladder, and a poorly functioning bladder.
There are four types of urinary incontinence:
Urinary incontinence is the inability to control urine flow.
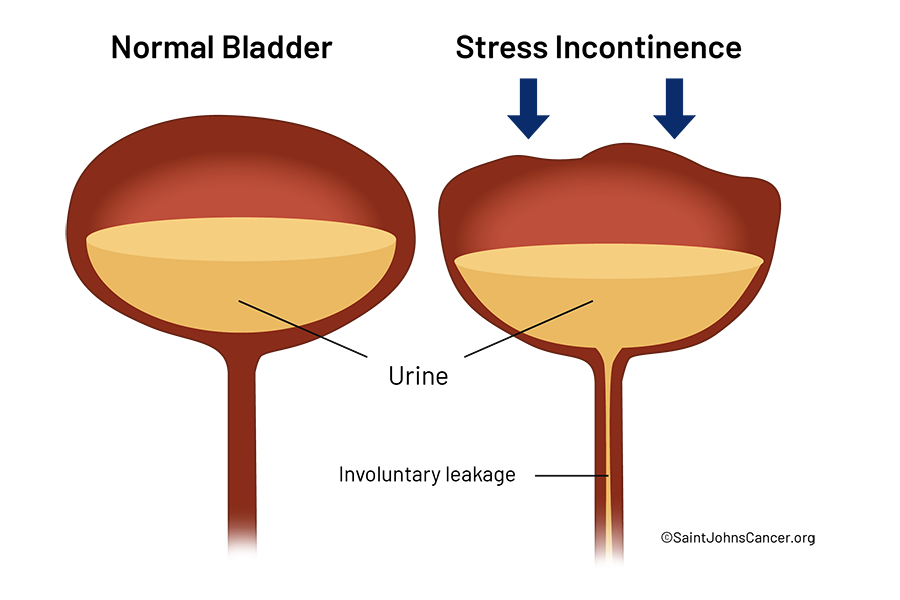
Stress Urinary Incontinence (SUI)
Pressure on the abdomen and pelvis, such as sneezing, coughing, laughing, or exercise, causes urine leakage.
Urge Incontinence
Sudden urge to urinate followed by leakage of urine.
Mixed Urinary Incontinence
Combination of both stress and urge incontinence.
Overflow Incontinence
Since the bladder is never completely empty, dysfunction causes periodic leakage of urine.
Overactive Bladder
Overactive bladder occurs later in life and is a common condition. It involves the sensation to void, or a bladder spasm to void, without stimulation from having a full bladder. There is a variety of causes from neurologic to hormonal.
Non-Obstructive Urinary Retention
This condition is characterized by the inability to completely empty the bladder that is not the result of blockage of the urinary channel. This is usually due to an underlying cause of bladder weakness. Individuals will have a weak stream when they urinate.
How do you diagnose voiding dysfunction?
- A urinalysis, cystoscopy (looking into the bladder to locate problems)
- Bladder scan (ultrasound of the bladder which measures the amount of urine left in the bladder)
How do you Treat Voiding Dysfunction?
Voiding dysfunctional is the irregularity of bladder or urinating function, which can be caused by a host of conditions involving urine storage (bladder), transfer (kidney to bladder, or bladder to ureters), or discharge from the body. Treatment can involve surgical and non-surgical techniques.

Non-surgical and Behavioral Treatment Techniques
Pelvic floor therapy is one of many treatments for voiding dysfunction. Medication, Kegel exercises, biofeedback (a type of therapy that uses sensors attached to the body), timed voiding, and bladder training are a few options used by urologists.
Injections
If lifestyle changes and prescription drugs are not a viable option, or the side effects of the drugs are intolerable, then botulinum toxin, better known as Botox®, may be an option. It is injected into the bladder muscle to help relax the contracting triggers of overactive bladder or urge incontinence. This treatment may need to be repeated in 3 or more months. Risks include infection and retention of urine.
Stimulating Nerves (Neuromodulation Therapy)
Neuromodulation therapy is a non-invasive treatment that uses electrodes to stimulate nurves through the surface of the skin to block pain signals. These electrical waveforms travel through tissue, muscle, and superficial nerves to achieve a therapeutic effect.
Sacral neuromodulation (SNS)
This treatment works by stimulating the sacral nerve (near the base of the spine) that connects to the bladder. SNS therapy basically uses a “bladder pacemaker” to interrupt these signals from the bladder to the brain, which can improve OAB symptoms like urgency and frequency. The device delivers electrical impulses to the bladder to essentially stop the signals from the spinal cord that cause OAB. Though rare, risks can include site infection, neuron damage, spinal cord bleeding, and rarely infection.
Percutaneous tibial nerve stimulation (PTNS)
PTNS is an out-patient, minimally invasive therapy that stimulates the tibial nerve. It is performed during an office visit and takes about 30 minutes. A small acupuncture needle electrode is placed in the ankle. Gentle electrical pulses are sent to the tibial and sacral nerves. The electrical pulses help block nerve signals that aren’t working correctly. PTNS typically requires a total of 12 treatments.
Surgery
Several minimally invasive procedures as well as more extensive surgical procedures may be necessary to treat voiding dysfunction. Robotic assisted surgery offers improved recovery time for patients while extending the capability of the surgeon working in the smallest of spaces. Your urologist will offer range of treatments available to you and can provide an out-comes based approach.
Urethral Injections for Stress Incontinence
Urethral injections for stress incontinence involves using bulking agents to improve urinary control. A urethral bulking agent is a material that the urologist injects into the wall of the urethra. It increases the amount of resistance in the urethra which helps prevent urine loss due to physical activities such as coughing, laughing, and exercise. Injections can be repeated every 3 months if needed. This method is not as effective as surgery but offers minimal downtime. Bulking agents are a temporary treatment.
Surgery for Women with SUI (Sling surgery)
Sling surgery is the most common treatment for women with stress incontinence. A small strip of synthetic mesh (or your own fascia) is placed under your urethra as a hammock to support the urethra.
There are two types of sling surgeries.
Midurethral sling
The midurethral sling is the most common type of surgery used to correct SUI. The sling is made out of a narrow strip of synthetic mesh that is placed under the urethra with a variety of techniques: retropubic, trans obturator and single-incision.
For sling surgery made from surgical mesh, the surgeon may only need to make a small cut (incision) in the vagina. The sling is then inserted under the urethra and anchored in the surrounding pelvic floor tissue. This surgery is short and recovery may be shorter than with an autologous sling. There are additional risks associated with using mesh that you should discuss with your surgeon.
Autologous sling
In this type of surgery, the sling is made from a strip of your own tissue (autologous) taken from the lower abdomen or thigh. The ends of the sling are stitched in place through an incision in the abdomen.
Bladder Neck Suspension (Retropubic Suspension)
Bladder Neck Suspension is also Colpo suspension, or Burch Suspension, which is usually performed at the time of a hysterectomy. In this surgery, sutures are placed in the tissue along the side of the bladder neck and urethra to support the urethra and sphincter muscles to prevent them from moving downward and accidentally opening. There are certain risks with this surgery and should be discussed with your doctor.
Surgery for Men with Stress Urinary Incontinence
There are a variety of treatments for men to address SUI including surgical techniques and medication.
Artificial Sphincter
The most effective treatment for male SUI is an artificial urinary sphincter device.
This urinary device has three parts:
- A fluid-filled cuff (the artificial sphincter), surgically placed around your urethra.
- A fluid-filled, pressure-regulating balloon, inserted into your belly.
- A pump you control inserted into your scrotum.
The artificial urinary sphincter cuff is filled with fluid which keeps the urethra closed and prevents leaks. When you press on the pump, the fluid in the cuff is transferred to the balloon reservoir. This opens your urethra, and you can urinate. Once urination is complete, the balloon reservoir automatically refills the urethral cuff in 1-3 minutes.
Artificial sphincter surgery can cure or greatly improve urinary control in more than 7 out of 10 men with SUI. Results may vary in men who have had radiation treatment. They also vary in men with other bladder conditions or who have scar tissue in the urethra.
Male Sling for SUI
The male sling is a narrow strap made of synthetic mesh placed under the urethra through small surgical incisions near the scrotum. As an outpatient procedure, the sling for males is used primarily for only mild SUI cases. It is less effective and not recommended in men who have had radiation therapy to the prostate, pelvis, rectum, or urethra. Risks including injury to urethra, bladder, urinary retention, mesh erosion or infection.
Oral Medications
Anticholinergics
Anticholinergic drugs work by blocking the action of a chemical messenger acetylcholine, so the bladder has less contractions.
Anticholinergic medications include:
- Oxybutynin (Ditropan XL, Oxytrol)
- Tolterodine (Detrol)
- Darifenacin (Enablex)
- Solifenacin (Vesicare)
- Trospium
- Fesoterodine (Toviaz)
Side effects include:
- Dry mouth
- Constipation
- Do not use if you have glaucoma
Mirabegron (Myrbetriq)
Can treat mostly urge urinary incontinence and overactive bladder. Mirabegron relaxes the bladder muscle and can increase the amount of urine your bladder can hold. It will also help to empty your bladder more completely because the bladder is holding more urine.
Side effects include:
- Nausea
- Diarrhea
- Constipation
- Dizziness
- Headache
- Increase blood pressure
Estrogen
Low-dose, topical estrogen in the form of a vaginal cream, that can rejuvenate deteriorating tissues in the vagina and urinary tract and relieve some incontinence symptoms.
Estrogen cream is not recommended if you have a:
- History of breast cancer
- Uterine cancer
- Deep Vein thrombosis (DVT)

Imipramine
Imipramine (Tofranil) is a tricyclic antidepressant. It relaxes the bladder muscle, while causing the smooth muscles at the bladder neck to contract. It may be used to treat mixed incontinence when there is both urge and stress incontinence.
Usually taken at night because it can cause drowsiness.
Side effects include:
- Irregular heartbeat
- Dizziness
- Fainting from reduced blood pressure
- Dry mouth
- Blurry vision
- Constipation
Duloxetine
Duloxetine (Cymbalta) is a serotonin and norepinephrine reuptake inhibitor that is approved to treat depression. Studies suggest it may also work for both urinary incontinence and depression.
Side effects include:
- Nausea
- Dry mouth
- Dizziness
- Constipation
- Insomnia
- Fatigue
If you have questions regarding voiding dysfunction or treatments, please call today, or Click Here to make an appointment.