Prostate cancer cases are reviewed by a multi-disciplinary tumor board at Saint John’s Cancer Institute and Health Center to personalize effective treatment plans.
What is Prostate Cancer?
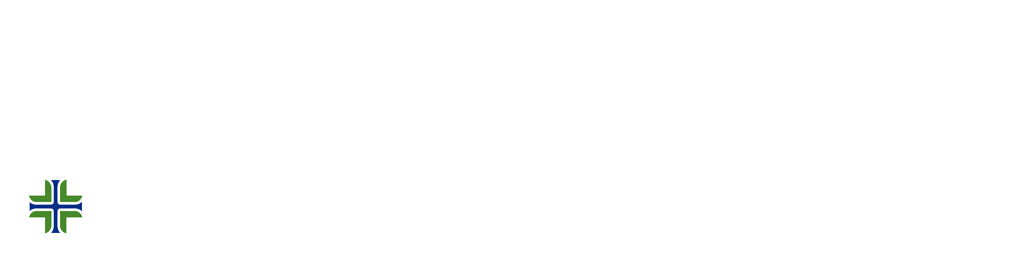
Prostate cancer develops in the prostate gland in males. It is the second most common cancer among men after skin cancer. Prostate cancer grows slowly, requiring minimal or no treatment, and is confined to the prostate gland. However, other prostate cancers are aggressive and can spread quickly to surrounding tissues and beyond.
Growths in the prostate can be benign or malignant tumors:
Benign Prostate tumors:
Tumors that are benign are not cancerous, and not a threat to life in most circumstances. Unlike cancerous tumors, they do not invade the surrounding tissue or spread to other organs. Once they are treated or removed, they usually do not grow back.
Malignant Prostate tumors:
Tumors that are malignant are cancerous. Although they usually can be surgically removed, they can also grow back. Untreated tumors can spread to other areas of the body, including organs such as the liver, colon, lung, etc. When this happens, cancer has metastasized, creating conditions for new tumors to form beyond the original site.
When prostate cancer is detected early, we have the best chance for successful treatment.
What are the Signs and Symptoms of Prostate Cancer?
In its early stages, prostate cancer may not cause any signs or symptoms, and is curable. More advanced prostate cancer may cause signs and symptoms such as:
- Trouble urinating
- Need to urinate more often, especially at night
- Decreased force in the stream of urine
- Blood in the urine
- Blood in the semen
- Bone pain
- Losing weight unexpectedly
- Erectile dysfunction
What are the Risk Factors for Prostate Cancer?
Though medical science does not have a definitive reason for what causes prostate cancer, several risk factors have been identified:
Age:
Prostate cancer is rare in men younger than 40. The risk rises after age 50. About 60 percent of cases occur in men over 65.
Race and ethnicity:
Prostate cancer occurs more often in African American men than in men of other races. White men are at greater risk of prostate cancer than Asian-American and Hispanic men.
Family history:
Prostate cancer seems to run in some families. Having a brother or father with prostate cancer more than doubles the risk of developing the disease.
Diet:
Men with diets high in red meat and low in fruits and vegetables have a higher risk of prostate cancer. A healthy diet may be the most practical way to reduce your risk of prostate cancer.
Obesity:
People who are obese may have a higher risk of prostate cancer compared with people considered to have a healthy weight. In obese people, the cancer is more likely to be more aggressive and more likely to return after initial treatment due to hormone and other physiological imbalances in the body that are less profound in those with normal body weight.
How is Prostate Cancer Diagnosed?
To reach a diagnosis of prostate cancer, a physical examination is performed while obtaining a thorough medical history. We will ask specific health questions, make note of the symptoms you may have experienced, and include any other pertinent information. One or more tests may be required such as a prostate-specific antigen (PSA) test.
The following tests may be used to diagnose prostate cancer or determine if it has spread:
PSA blood test
The prostate-specific antigen (PSA) blood test is one of the first tests used for men who have symptoms of prostate cancer, or for men seeking to perform routine health checks. Men with a PSA level between 4 and 10 have about a 1 in 4 chance of having prostate cancer. If the PSA is above 10, the chance of having prostate cancer is more than 50 percent.
What is a good PSA Level?
Normal PSA Levels for Men |
|
Age range |
Normal PSA range (ng/ml) |
| 40 – 49 | 0 – 2.5 |
| 50 – 59 | 2.6 – 3.5 |
| 60 – 69 | 3.6 – 4.5 |
| 70 – 79 | 4.6 – 6.5 |
Biopsy
Your urologic oncologist will obtain a sample of tissue from your prostate gland. A pathologist examines the tissue for signs of cancer. If cancer cells or a tumor are found, the pathologist grades the cancer level and provides a Gleason score. These scores range from 2 to 10. A higher-grade score indicates that cancer will grow faster and is more likely to spread.
Additional Tests
Your urologic oncologist may order other tests to help determine the stage of your prostate cancer:
- Bone scan: This test can help determine if cancer has spread from the prostate to the bones.
- CT scan: An X-ray machine linked to a computer can show whether prostate cancer has spread to the lymph nodes or other parts of the body.
- MRI: A machine that generates full-body imaging using a magnetic field instead of other technologies, such as X-ray. The waves generate detailed pictures that can show whether prostate cancer has spread to lymph nodes or other areas.
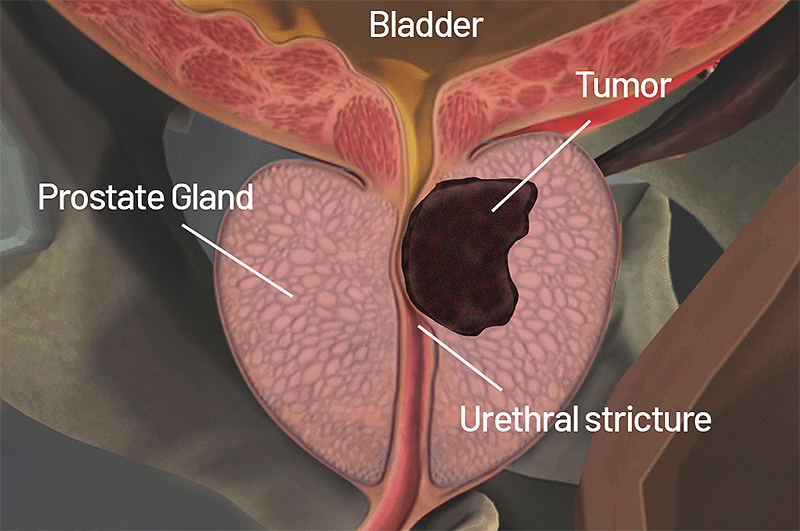
Targeted MRI/Ultrasound Fusion Biopsy
Targeted MR/Ultrasound Fusion Biopsy is becoming the new standard in prostate care. UroNav, a medical device by Philips, fuses pre-biopsy magnetic resonance (MR) images of the prostate with ultrasound-guided biopsy images in real time. This offers the best way to discern the prostate from suspicious lesions, providing the most powerful solution for analysis, planning, and targeted biopsy of the prostate. This approach consists of using DynaCAD software for Prostate and the UroNav fusion biopsy system–a comprehensive solution that offers cutting-edge imaging for patients with elevated and/or rising PSA levels.
The fusion of the MR and ultrasound images uses electromagnetic tracking, like your phone’s GPS system; a tiny tracking sensor attached to the trans-rectal ultrasound probe generates a small, localized electromagnetic field that helps isolate the location and orientation of the biopsy device. A sophisticated algorithm maintains the fusion of MR and ultrasound images, even if the patient moves.
Prostate Cancer Stages:
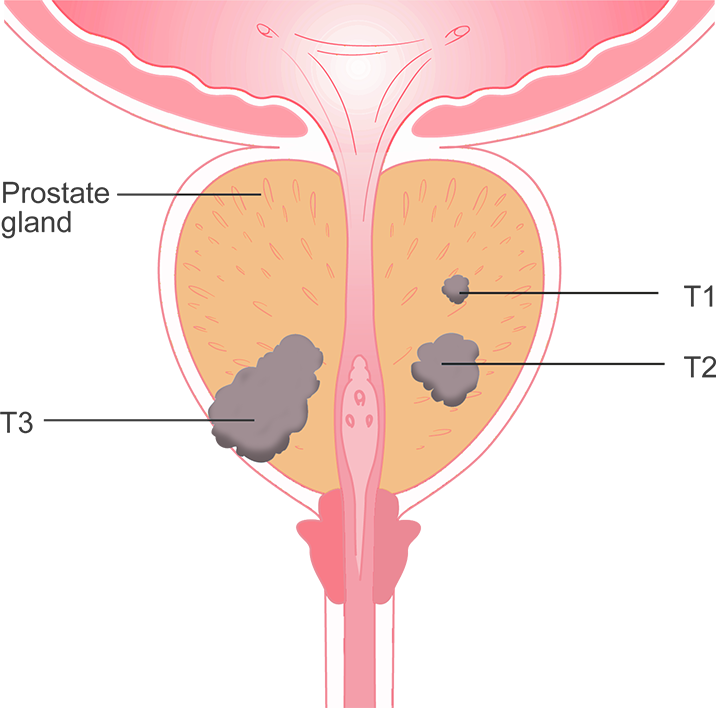
- Stage 1: The cancer is only in the prostate.
- Stage 2: The tumor has not spread beyond the prostate, but it is more advanced than Stage 1.
- Stage 3: The tumor has spread beyond the prostate, but it has not reached the lymph nodes.
- Stage 4: Cancer may have spread to the bladder, rectum, lymph nodes, bones, or other parts of the body.
Advanced Prostate Cancer Treatment
At the Saint John’s Health Center, we offer some of the most advanced treatments for prostate cancer throughout Los Angeles and Southern California.
Treatment Approach
You may receive more than one type of treatment, depending on several factors, including the grade of the tumor, where it is located, and whether it has spread to other parts of your body. Before we set up a specific treatment plan for your prostate cancer, we will take the following into account with an outcomes-based approach:
- Your age and overall health
- Medical and family history
- The extent of the disease
- Your tolerance for specific medicines, procedures, or therapies
- Expectations for the course of the disease
- Your treatment preference
Active Surveillance for Prostate Cancer
Your urologic oncologist may suggest Active Surveillance if your prostate cancer is in an early stage and growing slowly. Instead of immediate treatment, your doctor will check you regularly and perform tests to monitor your prostate cancer. Based on the progression, treatment may be delayed or may not be recommended. Our team will discuss the options available if treatment is needed so that you can make the best treatment decision.
Prostate Cancer Surgery
Depending on how advanced the cancer is, the urologic oncologist may remove part or the entire prostate and nearby lymph nodes. Removal of the entire prostate gland is called a radical prostatectomy. Surgery for prostate cancer usually requires an overnight hospital stay for monitoring. Once released from the hospital, there are typically no restrictions on activity after four weeks.
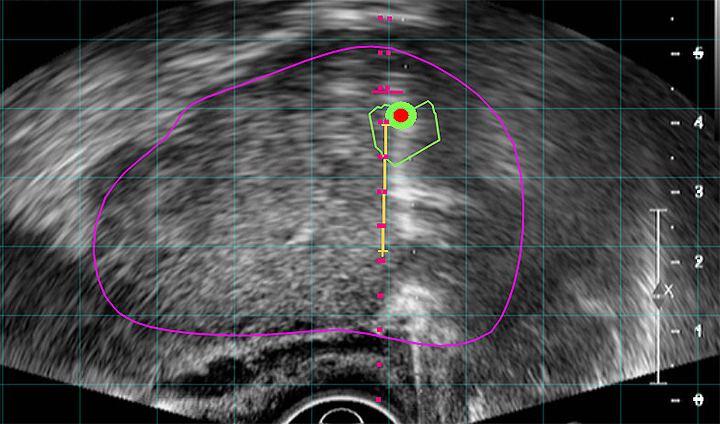
A minimally-invasive Approach
We specialize in robot-assisted, minimally invasive prostate surgery (prostatectomy) using the da Vinci Surgical System. In this procedure, the surgeon uses a console and 3D screen to control a surgical robot that transfers the doctor’s movements precisely. This minimally invasive surgery offers faster recovery and less time away from home.
Most prostate surgeries at Saint John’s Health Center are minimally invasive procedures, resulting in smaller incisions, less blood loss, less pain, and shorter recovery time. Our experience in successful prostate surgeries is of the top in the nation. Dr. Timothy Wilson is a pioneer in robotic-assisted prostate surgery.
Radiation Therapy for Prostate Cancer
Radiation therapy is an option for men with early-stage prostate cancer. It also may be used after surgery to destroy any remaining cancer cells.
There are two types of radiation therapy to treat prostate cancer:

External Beam Radiation
Computer imaging is used to target prostate cancer. This procedure allows for a modulated dose of radiation to the treatment area while reducing damage to surrounding tissue.
Low Dose-rate Radiation (LDR) or brachytherapy
Small radioactive sources (seeds) are inserted into the prostate, where they deliver a lower dose of radiation directly to the tumor. Over time, the radiation from the seeds wears off.
Prostate cancer radiation therapy can sometimes result in the injury of nearby healthy tissue, causing unwanted side effects such as bowel dysfunction. That’s why we now offer SpaceOAR Hydrogel, an innovative device aimed at helping to maintain quality of life and minimize side effects of radiation treatment by protecting nearby organs at risk during treatment.
Hormone Therapy for Prostate Cancer
Hormone therapy blocks male hormones, which can cause prostate cancer to grow. This treatment is used in advanced prostate cancer, or in combination with surgery or radiation therapy. In some cases, it includes surgery to remove the testicles, the body’s main source of testosterone.
Chemotherapy for Prostate Cancer
Chemotherapy kills fast-growing cancer cells and may be used to treat advanced prostate cancer. It is usually administered intravenously. Chemotherapy may be used to treat prostate cancer before or after surgery.
It may be used to help:
- Shrink the tumor before surgery
- Keep cancer from recurring after surgery
- Prolong life when surgery is not an option
High Intensity Focused Ultrasound using the Focal One Treatment System

Introducing Focal One: Non-invasive Robotic-Assisted Treatment for Prostate Cancer
Focal One is the world’s most advanced high-intensity focused ultrasound (HIFU) technology. This technology is available for men diagnosed with localized prostate cancer.
With Focal One, our surgeons can locate the contours around the diseased tissue and destroy the tumor with high-intensity ultrasound waves. This procedure reduces the risk of damaging healthy tissue and minimizes side effects. HIFU is customized for each patient, preserving the prostate while aiming to maintain your quality of life.
See High Intensity Focused Ultrasound (HIFU) for Prostate Cancer
See Focal One Frequently Asked Questions (FAQs)
Focal One Videos
If you have questions regarding prostate cancer treatments, your Gleason score, or PSA, please call today.