What is Lung Cancer?

Lung cancer is a malignant disease characterized by the uncontrolled growth of abnormal cells in the tissues of the lungs. It is one of the most common and deadliest forms of cancer, with a significant impact on both men and women. The incidence of lung cancer has been historically higher in men than in women; however, this gap has been closing due to changing smoking patterns and increased exposure to risk factors in both sexes.
It is one of the most prevalent and deadly forms of cancer globally, primarily caused by long-term exposure to harmful substances, especially tobacco smoke. Symptoms of lung cancer can include persistent cough, chest pain, shortness of breath, unintended weight loss, and coughing up blood. In recent years, advancements in research have led to a better understanding of the underlying molecular mechanisms of lung cancer, enabling the development of more targeted and personalized treatment strategies.
Understanding Risk and Symptoms of Lung Cancer
Prevention remains a crucial aspect, with efforts focused on prevention, such as reducing tobacco use and carcinogenic exposure, as well as promoting awareness of the importance of early screening and detection to improve outcomes for those at greast risk.
How does lung cancer differ between men and women?
Lung cancer has historically been more prevalent in men, but the gap has been narrowing over the years. This is largely due to the increased adoption of smoking by women in the latter half of the 20th century. As a result, the occurrence of lung cancer in women has risen, highlighting the importance of understanding and addressing this disease in both genders.
Overall, the chance that a man will develop lung cancer in his lifetime is about 1 in 15; for a woman, the risk is about 1 in 17. Black men are about 15% more likely to develop lung cancer than white men while the rate is about 14% lower in black women than in white women. Both black and white women have lower rates than men, but the gap is closing. The lung cancer rate has been dropping among men over the past few decades, but only for about the last decade in women.
Who is most at risk of developing lung cancer?
While anyone can develop lung cancer, certain factors can increase the risk. The primary risk factor for lung cancer is smoking, with approximately 85% of lung cancer cases linked to tobacco use. Other risk factors include exposure to secondhand smoke, environmental factors such as air pollution, exposure to carcinogens in the workplace (like asbestos, radon, and certain chemicals), a family history of lung cancer, and certain genetic mutations.
You can also develop lung cancer from breathing second-hand smoke or from exposure to cancer-causing substances such as:

- Radon, which naturally occurs outdoors in harmless amounts, but sometimes becomes concentrated in homes built on soil with natural uranium deposits.
- Asbestos
- Chromium
- Nickel
- Radioactive ores, such as uranium and plutonium
- Arsenic
- Vinyl chloride
- Silica
- Coal products
- Chloromethyl ethers
- Diesel exhaust
- Air pollution and soot
- Tar
What are the Signs and Symptoms of Lung Cancer?
The symptoms of lung cancer can vary, and they may not become noticeable until the disease has progressed to advanced stages. Common symptoms include persistent coughing, coughing up blood, chest pain, difficulty breathing, unexplained weight loss, fatigue, hoarseness, and recurrent respiratory infections.
Signs and symptoms of lung cancer may include:

- Cough that doesn’t go away and worsens over time
- Trouble breathing
- Chest pain
- Wheezing
- Coughing up blood or rust-colored mucus
- Hoarseness
- Loss of appetite
- Weight loss for no known reason
- Feeling very tired
- Pneumonia or bronchitis
- Shoulder pain
- Bone pain
- Yellowing of skin and eyes (jaundice)
- Headache, seizures, or confusion
- Enlarged lymph nodes in the neck
Types of Lung Cancer
Lung cancer is broadly categorized into two main types: small-cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC). NSCLC is the most common type, and it includes several subtypes, with the most prevalent ones being squamous cell carcinoma, adenocarcinoma, and large cell carcinoma.
Non-Small Cell Lung Cancer
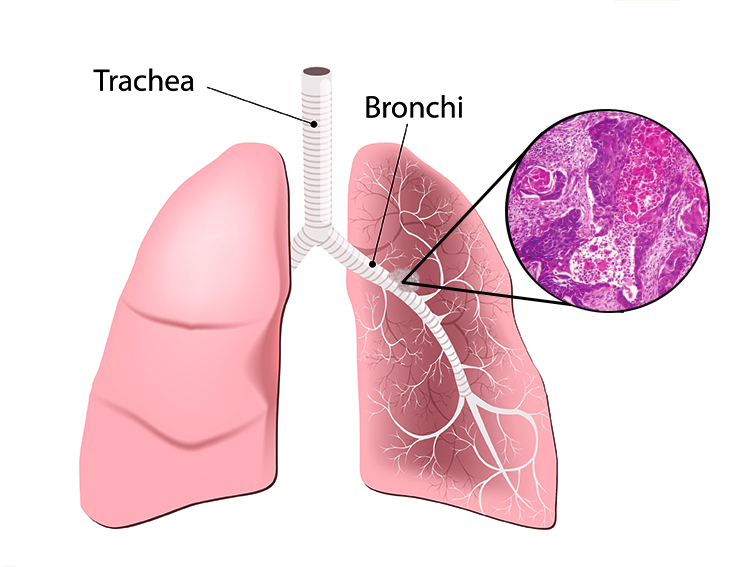
This type of NSCLC typically originates in the lining of the bronchial tubes. It is often associated with a history of smoking and is more common in men. Squamous cell carcinoma tends to cause symptoms earlier in the disease progression.
Adenocarcinoma
Adenocarcinoma arises in the cells that produce mucus in the lining of the airways. It is the most common type of lung cancer in both men and women, and it often occurs in nonsmokers or former smokers. Adenocarcinoma is more likely to develop in the outer parts of the lungs.
Large Cell Carcinoma
This type of NSCLC tends to grow and spread quickly. It can appear in any part of the lung and is often associated with a poor prognosis.
Small Cell Lung Cancer
Small cell lung cancer is sometimes called oat cell cancer. It grows rapidly and spreads to other organs. There are two types:
Limited cancer is generally found in one lung. There may be cancer in nearby lymph nodes on the same side of the chest.
Extensive
Extensive cancer has spread beyond the primary tumor in the lung into other parts of the body.
Lung Cancer Diagnosis

Diagnosis often involves imaging tests such as CT scans and X-rays, biopsies, and other procedures to determine the type and stage of the cancer. Typically, lung cancer screening is offered to older adults who are at greatest risk, such as those who have smoked heavily for many years or who have quit in the past 15 years having smoked at least a pack a day for 20 years (20-pack years). See Screening for more information.
You will need to discuss your lung cancer risk and decide whether lung cancer screening is appropriate. If you have reason to beleive you may have lung cancer, we will recommend one or more tests to identify if cancer is present and rule out other conditions.
Testing for lung cancer may include one or more of the following:
Blood and urine tests for cancer
The Saint John’s Cancer Institute is a leader in liquid biopsies (checking a patient’s blood to look for cancer cells). We are studying the use of these tests for diagnosis, staging, and follow-up.
Sputum cytology
Looks for cancer in sputum tests.
Thoracentesis
A needle passes between the ribs into the chest cavity to drain fluid which can be checked for cancer cells.
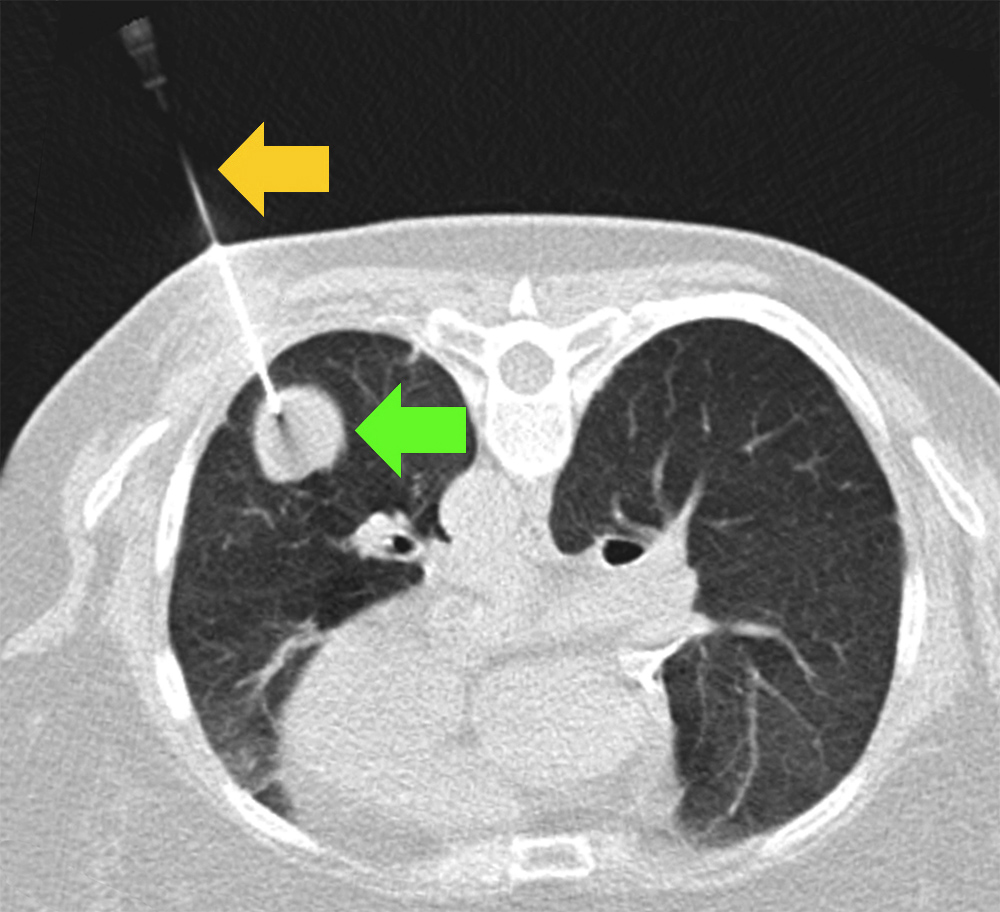
Needle biopsy
A needle guided by a CT scan passes between the ribs into a lung mass. Tissue is evaluated under a microscope.
Surgical biopsy
Often performed by video-assisted thoracic surgery (VATS) under general anesthesia, is obtained through a small incision in the chest. A video camera is inserted so the surgeon can see what to biopsy. The patient usually stays in the hospital for 1-2 days. Sometimes the procedure is expanded to remove the whole mass for a cure.
Bronchoscopy
A flexible tube (bronchoscope) passes into the trachea to look for narrowed windpipes or tumors, and to get biopsies.
Navigational bronchoscopy
Uses a computer as a GPS guidance system to direct the bronchoscope where to get a biopsy
Transbronchial biopsy
Uses fluoroscopy to direct the bronchoscope where to get a biopsy
Endobronchial ultrasound (EBUS)
Uses ultrasound to direct the bronchoscopy where to get a biopsy of lymph nodes or lung masses.
Mediastinoscopy
Under general anesthesia, an instrument called a mediastinoscope passes into the mediastinum to obtain biopsies of mediastinal lymph nodes.
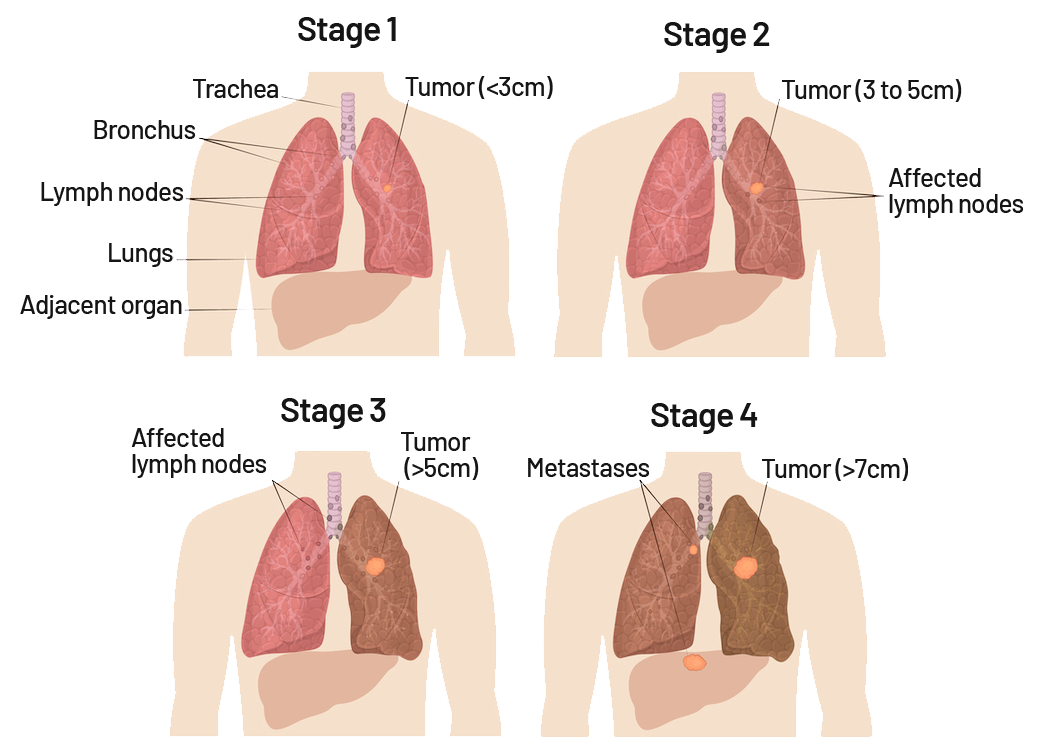
What are the Stages of Lung Cancer?
Lung cancer is staged based on the size of the tumor, the extent of its spread to nearby lymph nodes or other organs, and its overall metastasis. The stages range from Stage I (localized disease) to Stage IV (advanced and metastatic disease). In early stages, lung cancer typically does not reveal significant symptoms. Symptomatic lung cancer typically occurs when the disease has advanced. If lung cancer has metastasized to a nearby organ, such as the liver, the cancer now developing within the liver is still considered lung cancer. Therefore, medical treatments that are specifically designed for lung cancer will continue to be used to fight the cancer in the liver.
The Occult stage of lung cancer is when cancer cells can be identified in mucus or other liquid biopsy though the tumor can’t be seen on imaging scans or a biopsy. Occasionally, lung cancer is identified at stage 0, where the tumor can be seen on imaging scans but is very small.
Lung Cancer Stages 1-4
- Stage 1: The cancer is localized and has not exceeded 3cm in diameter nor detected in the lymph nodes.
- Stage 2: The cancer may spread to nearby lymph nodes but has not grown to exceed 5cm.
- Stage 3: The cancer has spread further into your lymph nodes and has exceeded 5cm.
- Stage 4: The cancer has spread to other parts of the body including other organs and has grown to 7cm or larger.
Lung Cancer Treatment Summary
Treatment options for lung cancer depend on the type, stage, and overall health of the patient. Treatment modalities may include surgery, radiation therapy, chemotherapy, targeted therapy, immunotherapy, and palliative care to manage symptoms and improve quality of life. The choice of treatment is personalized based on individual factors.

Lung Cancer Surgery
Surgery is a common method to remove the tumor from the lung or remove a portion of the lung so that the remaining organ can funtion more effectively. This is optimal if the tumor site is confined to an area of the lung while the remaining part of the lung is in good health and functioning well.
Radiation Therapy
Radiation therapy (or radiotherapy) is a medical treatment that uses high-powered energy rays such as X-rays or protons to destroy cancer cells and shrink tumors. Radiation therapy is an option for many cases of cancer when other treatments aren’t possible or if they haven’t helped.
Chemotherapy
Chemotherapy uses drugs to kill rapidly growing cells, including cancer cells. Chemotherapy can be administered intravenously (through a vein), in pill form, or both. Advancements in chemotherapy can target specific parts of cancer cells, which provides very predictable results.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities that are present within cancer cells. By focusing on these abnormalities, targeted drug treatments can block cancer progression and cause cancer cells to die.
Learn more
Click here for Lung Cancer Treatment.
Prevention and Lung Cancer Screening
The most effective way to prevent lung cancer is to avoid smoking and exposure to tobacco smoke. However, there is a big misconception that only smokers can get lung cancer. You can also develop lung cancer from breathing secondhand smoke or from exposure to cancer-causing substances. For those who have quit smoking, the risk of lung cancer decreases over time. Additionally, reducing exposure to environmental pollutants and maintaining a healthy lifestyle, including regular exercise, can help lower your risk. Click here to learn more about our lung cancer screening program.
3 tips for stopping smoking:
- Don’t go alone: There are online, virtual, and in-person smoking cessation groups. All have proven beneficial to help patients quit smoking.
- Pay attention to your smoking triggers and try to avoid them: Are you most likely to smoke while having a glass of wine with friends? Meet for a walk instead. Or maybe you smoke at work when you’re stressed. Instead of heading outside, try a meditation app. Once you pinpoint your smoking triggers, replace them with new habits to make quitting easier.
- Hit the Gym: Exercise has been shown to help stave off nicotine cravings—and it can help reduce weight gain, which can sometimes be an unwanted side effect of quitting smoking. Win-win!
Lung cancer screening is crucial, especially for individuals at high risk, such as current or former heavy smokers. Screening tests, such as low-dose CT scans, can help detect lung cancer at an earlier stage when it’s more treatable.
Call today to learn more about Lung Cancer Symptoms and Diagnosis. Our multi-disciplinary team is ready to support you.
If you have questions regarding Lung Cancer Screening or Treatment, please call today. Click here to request an appointment.